Facts and Fiction: Fiber with Crohn’s or Ulcerative Colitis
Facts about Fiber for IBD
The topic of dietary fiber has been on my mind to write about for a while now as I’ve continued to notice a number of people with IBD that I talk to that are scared to include fiber in their diet.
This fear isn’t unfounded either, sometimes living with IBD can make all sorts of traditionally healthy foods feel painful.
However, as I’ve described in previous blogs breaking down the different types of remission, just because something triggers symptoms does not mean it’s triggering inflammation.
The opposite could also be true!
Just because something isn’t painful, doesn’t mean it isn’t contributing to inflammation in the long term.
Confusing right?
The internet doesn’t help either, given that it is spreading fear around food choices for IBD that are misleading and often lacking scientific basis.
Some examples include:
- “All IBD patients should be on a low residue diet”….
- “Fiber causes stricturing and blockages in IBD”….
- “IBD patients shouldn’t eat (popcorn, berries with seeds etc) ever again”…
- “All IBD patients shouldn’t have leafy greens”…
The last two statements especially make me so sad. I can’t and don’t want to imagine a life without berries and greens!
And I’m guessing you probably wouldn’t either, yet these messages are so widespread that even practitioners and doctors are repeating them to patients.
As an IBD specialist and Dietitian, I aim to always stay open to new ideas that challenge my own since I know the science in this space is continually evolving.
So what did I do?
A little evidence search to see if anything has changed that I didn’t know about… and guess what?!
None of the above statements are true or have any scientific basis.
In fact, with most of them the research supports the opposite!
So now it’s time to set the record straight on fiber by going through the most misunderstood things about it as it relates to IBD.
Fiber with Crohn’s or Ulcerative Colitis
This blog post will describe all things fact and fiction about fiber! From different types of fiber, fiber supplements, low residue diets for IBD, nuts and seeds for IBD, and so much more! Keep reading to learn more.
Fact – There are Different Types of Fiber
All fiber is not the same, there are many different types of fibers and they vary a lot in terms of how they support our bodies.
Soluble Fiber
Soluble fiber is a type of fiber that absorbs water forming a gel in the digestive tract. This gelling action helps soak up excess moisture making it great for those suffering with diarrhea.
Soluble fibers are also excellent prebiotics that help feed our butyrate producing gut bacteria.
Butyrate aids in reducing inflammation in our digestive tracts and repairing any damage present.
Psyllium seed (not to be confused with the husk) is a good example of a soluble fiber.
SunFiber as found in our GutLove is also a great example! It is tasteless and completely dissolves in water so you can easily add it to tea or coffee.
Insoluble Fiber
Insoluble fiber doesn’t dissolve in water or absorb water but is important for removing things we don’t need hanging around in the digestive tract.
Insoluble fiber can increase transit time or movement through the digestive tract. Insoluble fibers are still consumed by bacteria further down in our digestive tract.
Psyllium Husk (not to be confused with the seed mentioned above) is a great example of an insoluble fiber.
The peels on fruits and vegetables are also examples of insoluble fibers.
Bottom line: I only named two types of fibers here. But there are several different types of fibers and they operate differently. There are even supplements one can include which we will talk about next.
Crohn’s Disease and Ulcerative Colitis Fiber Supplements
One of my favorite products is GutLove which contains SunFiber- one of the best tolerated prebiotics that’s really easy to incorporate into smoothies, tea, or water.
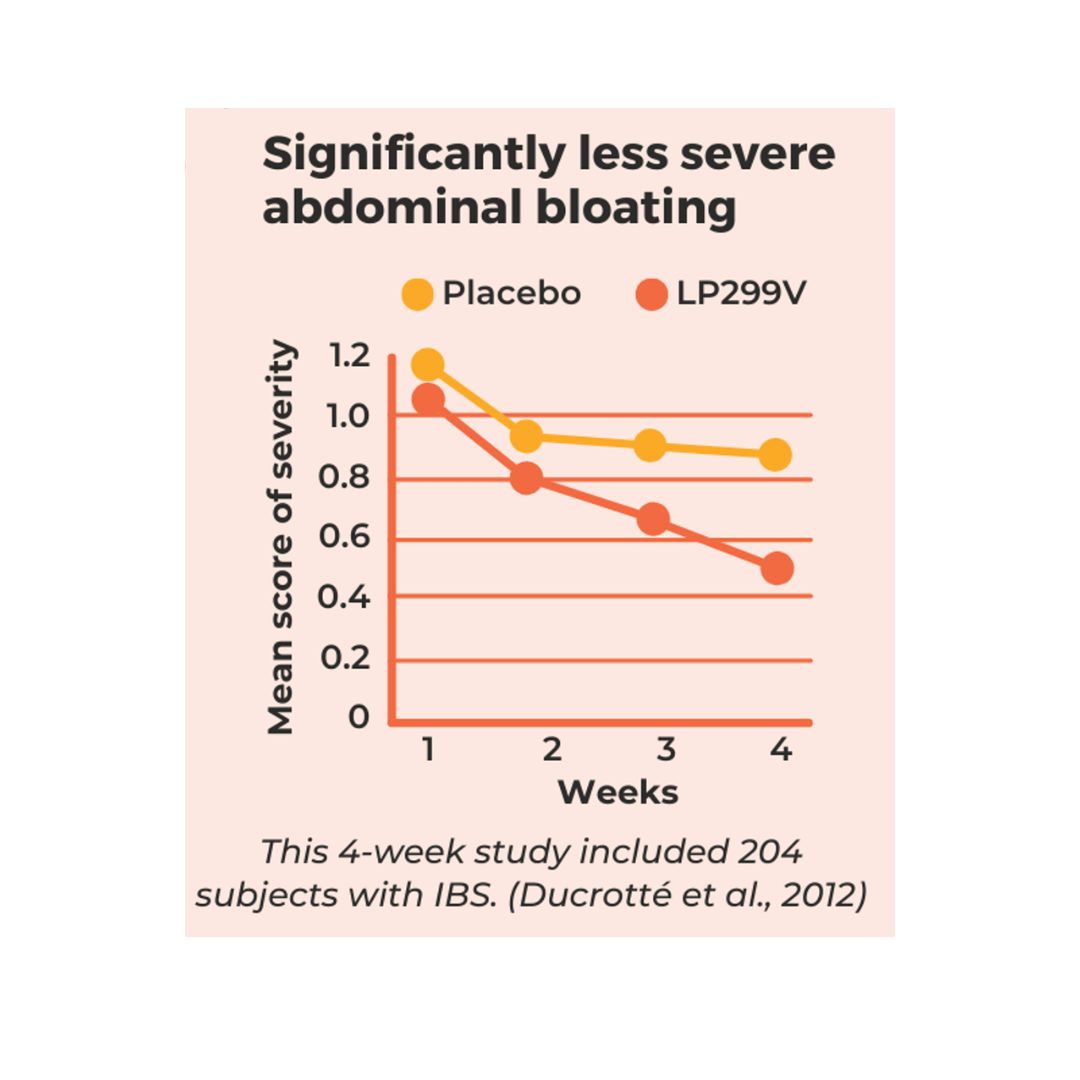
It’s also my favorite product because I’ve had the best success with helping to regulate bowel movements of those with Crohn’s and Ulcerative Colitis as it helps with constipation diarrhea, and reduces symptoms like gas and bloating (1).
Another bonus to using SunFiber is that it is also helpful in improving absorption of minerals like calcium, iron, zing, and magnesium.
Another supplement to consider is psyllium seed (not to be confused with psyllium husk). This is a gelling prebiotic similar to SunFiber that helps with supporting the growth of our helpful gut bacteria (2).
A study of 105 people with UC was conducted. Psyllium seed powder was given for 12 months and they saw some pretty cool results! After 12 months, of those taking mesalamine and psyllium seed powder, 70% were in remission. Those taking psyllium seed powder alone compared with just mesalamine – 60% stayed in remission compared to 65% in the mesalamine group (3).
Fiction – You should Eat A Low Residue/Fiber Diet
You might be surprised to learn that no reputable organizations in the world of IBD say to eat low fiber to support inflammation reduction! In fact, most say the opposite.
In fact, Crohn’s Disease patients who reported that they did not avoid high fiber foods were 40% less likely to have a disease flare up than those who avoided high fiber foods (4).
Not to mention, low fiber intake is actually a risk factor for both the development of Crohns and Ulcerative Colitis (5).
Low fiber intake is also a risk factor for the development of colorectal cancer (6).
So why then is a low residue diet or bland diet so commonly recommended to IBD patients?
While there are some scenarios where you might need to switch up the types of fiber in the diet to minimize blockage risk, improve tolerance, or to manage strictures (read more about that here), not including fiber at all can put you at risk for a flare up.
Fiber is an important fuel source for our most helpful gut bacteria present in the gut. And consumption of it helps our gut bacteria to produce more butyrate.
Increasing butyrate in the digestive tract can help with reducing inflammation locally in the digestive tract and systemically throughout the body (4).
Increasing butyrate is also helpful for improving and even helping to repair damage to the digestive tract lining (4).
The USDA currently recommends 25 grams per day of fiber for women and 38 grams per day for men under 50.
Bottom line: A low fiber or low residue diet isn’t ideal for the long term. If you aren’t handling fiber well, start by adding in soluble gelling fibers like sunfiber, or psyllium seed powder (not the husk). Root vegetables like zucchini and other squashes can also be a great starting place. Smoothies are also a great way to bring in easier to tolerate fibers. For a video on the research- check out our latest and click here.
Fact – Reducing High Fructose Containing Foods May Help in Some Crohn’s Patients
So I know you are thinking… What about the low FODMAP diet?
Believe it or not, there are relatively few studies on the low FODMAP diet for IBD.
There was one study where Crohn’s patients were asked to follow a low FODMAP diet. Overall, abdominal pain, bloating and gas did decrease with the diet in 56% of participants. Nausea, fatigue and reflux didn’t change (5).
At first glance, the data suggests that some Crohn’s patients who suffer from digestive symptoms (while in remission) can benefit from a low FODMAP diet.
If you looked at this study alone, you might try out a low FODMAP diet too.
However, we also know that over half of those with Crohn’s struggle with fructose malabsorption.
Knowing this, if 61% of people with Crohn’s struggle with fructose, they will also see improvements with this type of diet, but could just be related to fructose rather than all high FODMAP foods (6).
Therefore, instead of limiting all fermentable fibers, a Crohn’s patient could try out simply reducing high fructose items in the diet.
Some examples of high fructose foods would be honey, agave syrup, some juices, high fructose corn syrup and apples. Working with a dietitian on a lower fructose diet can be helpful in clarifying what the biggest triggers are.
Bottom line: While the low FODMAP diet might decrease symptoms in some people, this doesn’t necessarily correlate with lowered inflammation which is why I don’t recommend it to IBD patients. Also, based on the research, I suggest it’s the fructose rather than all fodmaps triggering symptoms.
Fiction – You Will Benefit From Avoiding Most Fiber-Containing Foods
Maybe you’ve tried a low residue diet before and seen reduced symptoms. And now you might be wondering what’s that all about?
Low residue diets typically are referred to as “bland” diets or those with very little fiber.
While you may potentially notice some decrease in symptoms, this doesn’t correlate with decreased inflammation or disease activity.
You can also have limited symptoms and still have ongoing inflammation. This is why relying on symptoms alone isn’t reliable. If you’d like to learn more about the different types of remissions- check out my blog here.
Bottom line: Including some fibers in the diet can actually help provide an anti-inflammatory affect through reducing inflammation and disease activity- this is why it’s so important to keep them in the diet. As mentioned previously, change the way you consume the fiber before taking it out completely!
Fact – You CAN Eat Nuts/Seeds
This might also surprise you, but there is no evidence supporting Crohn’s and UC patients can’t have nuts or seeds!
However, I hear on a weekly basis the many fears about nuts and seeds through things people have read online.
What we do know about nuts and seeds is that sometimes it’s the particle size of the food that can cause irritation, not the food itself.
What does this mean?
Simply changing the format of a food can help build tolerance.
For example:
- Instead of raw nuts and seeds, try nut or seed butter
- Instead of raw spinach, try spinach in a smoothie
Bottom line: If you find you struggle with fruits, vegetables, nuts or seeds- try consuming them a different way! Reducing the particle size of the food can make digesting them way easier.
A Final Note On Fiber During Flares & Remission
I know it can feel so confusing when navigating nutrition for Crohn’s and UC. You might be curious about the amounts of fiber needed to support your gut – or even be wondering how it’s possible to consume any without symptoms!
You might be in a flare and not sure what’s truly triggering (maybe it’s common gut triggers like caffeine, dietary fats, spicy foods, or sugar alcohols) or is it IBD…
You might also be in a place of unsure how to add fiber back in after years of being on a low fiber diet…
You might even be curious about if there are supplements that can help…
Just know that you don’t have to do it alone!
We have worked with hundreds of IBD patients each year on expanding their diets. Many leave able to consume foods they previously thought were totally out of reach.
Most of all – people report relief around finally getting clear guidance and a plan they feel confident in.
Recently one of our patients that worked with us mentioned:
“I’ve finally been able to start running again (something I always loved) without my IBD getting in the way and I’ve been surprised at how many foods I thought were triggers are actually not at all!”
Also, after working with us one of our other patients said:
“I just wanted to tell you how well things have been going this pregnancy. I have maintained my level of stability and digestive health from before the pregnancy, if not improved it! I am so thankful not to be struggling with digestion and not knowing what to eat to make things better. I am only 15 weeks in, but I think by this time in previous pregnancies I was already experiencing issues, so I’m really hopeful for continued good health this time around. And I’m thoroughly enjoying eating such a diverse diet compared to what I was stuck on for the year before I came to you.”
My hope for all Crohn’s and Colitis patients is for you to have more peace with food through getting quality evidence based nutrition guidance.
If you are struggling to have a diverse, fiber rich diet without triggering lots of symptoms – you aren’t alone. This is a common issue with IBD – but this is also what we are great at helping people navigate! We love helping people expand their diets and finally have the tools to reduce symptoms like bloating, abdominal pain, diarrhea, fatigue and more.
If you are skipping meals to avoid triggering symptoms – please know that you don’t have to do it all alone. We would love to help! If you are skipping meals – this puts you at risk for malnutrition which can impact how well you respond to medications.
If you need help getting there- I’ve got you covered! Want to work with a registered dietitian specialized in IBD? Set up a call here to learn how you can start.
Other blogs to check out:
To read more evidence-based IBD-related blogs, we have a new one on the Top 10 IBD Myths!
Got Ulcerative colitis UC and want to read up on UC nutrition? Check out our blog on What to Eat with Ulcerative colitis





Psyllium Husk is a soluble fiber. It is not insoluble.
Yes that is true, psyllium husk is about 50% insoluble with some soluble in it also. Psyllium seed however is mostly soluble. Two different fibers but same plant.
I have suffered for UC for the past 18 Years, and I am currently 54YO. I first contracted UC after giving up smoking. I have had 4 major flares in the past 18 years, all of which have required hospitalization. I am currently a non smoker.
I am currently in remission from my last flare which was the most severe yet and required 3 weeks of hospitalisation to bring it under control. I am now in remission.
I have always managed my condition currently without medication (unless I am having a severe flare in which case I have been hospitalised and medicated) and I am using the recommendations on this website to help manage my condition.
I currently use psyllium seed powder (as per recommended by this site) and slippery elm inner bark daily. I also use a product called Sunfiber by California gold nutrition which is partially hydrolised guar gum and appears to be the same as GUT LOVE.
My confusion is that most of the information that I find about psyllium husk states that it is a soluble fibre. As a matter of fact most sources claim that the husk of the psyllium seed contains the bulk of its soluble fibre. However on this website, it claims that psyllium husk is actually an insoluble fibre. The nutritional breakdown of most pure psyllium husk products list the total of 80% soluble fibre and 20 % insoluble fibre which seems to make it clear that pysllium husk is undeniably a soluble fibre, contrary to the information provided above.
So Im now confused- why is this website using psyllium husk as an example of insoluble fibre when it appears that it is the opposite? PLEASE EXPLAIN?
Also, it is very difficult to source psyllium seed powder as opposed to the psyllium husk which is commonly available. Will the husk powder be effective to help control my UC, or does it have to be the pyllium seed powder…?
Kind Regards
Marco
Gut love is a mix of two ingredients – so not the same, but yes it also has PHGG. Most psyllium husk is a mix of soluble and insoluble! So it’s both. Psyllium seed is mostly soluble though – so all of this just depends on which part of the psyllium you are referring to.
I can’t speak to what’s right for you off of a blog, but if you are interested in becoming a patient – please reach out.
I live somewhere (in Canada) where it’s very hard to find proper on going medical care. I’m finding it very difficult to get answers as to what kind of fiber supplement I’m supposed to take. I was given the suggestion of one that costs too much, but I’m not getting any guidance as to what I can use instead and the alternative I chose seems to be aggravating things.
Is there much of a difference between brand name supplements and store brand or no-name quality-wise, at least? I paid a full $10 less for the most recent supplement I bought, but like I said it’s aggravating things so if it means I have to scrape together that extra $10 every month or whatever, then so be it but I’d rather not.
what about trying food based fiber?
Why no husk but yes to psyllium seed?
the psyllium seed is rich in soluble fibers – we use both but for different things!
I was told after by a Dr., who didn’t recommend actually doing it, that some people go into remission by smoking
There is one study that looked at that and found those who already were smoking had some benefit to it… at the same time though there are so many huge downsides to smoking. To me, the huge risk outweighs the benefits!
Hi Ashley, love your approach, many thanks for the advice, it’s not an easy thing to cope with. I’m trying the soluble fibre as you suggest, could you tell me roughly how much psyllium seed I should use per day please? Best regards Jonny.
Thank you Jonny! You are so right, it’s not easy. I can’t provide individualized advice without knowing your case specifically but feel free to reach out and schedule a call!
All the comments that if someone reacts badly to some fibers, it might just actually be fine because it’s just causing symptoms and not inflammation are so dismissive! IBD symptoms can be absolutely quality of life destroying.
Thank you for bringing this up, I can see how it might come across this way. You are absolutely right- quality of life is so important for IBD. We always try to help people with symptom reduction. I find it a relief to know that not all symptoms are driven by an inflammation flare up personally- which is probably why I share it often. But I definitely didn’t intend it to be dismissive.
So glad to hear that I have more chooses of food to eat. So confusing. Some say don’t eat this or that and the next read says yes you can have that. So thanks for your information.
You are very welcome… we want to make things less confusing for people so I’m glad you are feeling relieved by the post!
The winning Powerball ticket worth an estimated $316.three Million ($225.1Million money) was sold in Green Bay, Wisconsin.
my blog post 파워볼분석기