Living with Microscopic Colitis – and any kind of inflammatory bowel disease like Crohn’s Disease or Ulcerative Colitis- can feel like a continuous game of roulette; never quite knowing when symptoms will appear or which foods will trigger symptoms, not to mention the emotional impact of it all.
Often it’s knowing what you are dealing with initially which will enable you to manage the condition more effectively. Here we look at what Microscopic Colitis is, what the causes and triggers may be, and which dietary changes you can make to reduce the symptoms.
What to Eat for Microscopic Colitis
What is Microscopic Colitis?
Microscopic Colitis is a type of inflammation of the colon or large intestine, that can cause watery diarrhea and cramping. While in microscopic colitis we don’t see bleeding, fistulas, or other complications common in other IBD’s- it can still be uncomfortable, painful, and unpleasant.
There are subtypes of the disease which include Collagenous Colitis and Lymphocytic Colitis; the symptoms and treatment of which are all the same.
What are the symptoms?
It may be that you already have a diagnosis of having the condition, however, if you are unsure and yet to find out if you might have Microscopic Colitis then it can be useful to know what the symptoms are:
- Watery, non-bloody diarrhea
- Diarrhea which occurs at night
- Abdominal pain
- Unexplained weight loss
- Fatigue
- An urgency to empty your bowels
- Fecal incontinence (urgency/not making it)
Symptoms can appear gradually or suddenly, worsening over time. They may differ in severity, and you may experience periods of remission when symptoms reduce or disappear and then return.
What can cause Microscopic Colitis?
It’s one thing knowing that you have a condition, it’s another knowing how to manage it. Often the best way to begin to treat a disease is to understand it first:
- In many cases, Microscopic Colitis is caused by abnormal immune reactions which leads to inflammation in the colon.
- People with certain immune disorders such as Rheumatoid Arthritis and Celiac Disease Type are more likely to develop the disease.
- It is thought that certain genes may be linked to having the disease, therefore Microscopic Colitis is not always preventable.
However, there are lifestyle factors that can play a part in developing the condition which can be monitored or eliminated. The following medications can be a risk factor:
- NSAIDS
- Acid blocking medications
- SSRIs, which is a type of antidepressant medication (Selective Serotonin Reuptake Inhibitors)
Smoking also greatly increases the severity of the disease. Other risk factors can include bile acid malabsorption when too much bile gets into the colon, microbiome changes, female hormones, and infections.
Lifestyle changes to manage Microscopic Colitis
There are a few changes you can make to reduce the level of discomfort and amount of flare-ups you might have, some of which may need support from specialists in that field:
- Check for Celiac Disease – Up to 50% of those with microscopic colitis have Celiac Disease and need to eliminate gluten by following a gluten free diet – ask your doctor if you’ve checked for Celiac Disease. There is both a blood test and endoscopic assessment to test for Celiac that your doctor may recommend.
- Stopping smoking – speak to your GP, local Pharmacy, or a Smoking Cessation Advisor to find the best way of quitting for you.
- Making key dietary changes – reducing caffeine, dairy, and alcohol are highly recommended to help reduce inflammation, as well as adding more pre and probiotic foods into your diet. You could speak to a dietitian or your GP to put an effective plan in place.
- Reducing inflammation in the gut – reducing or changing medications, under the guidance of your GP, while making the dietary and lifestyle changes recommended above.
- Bulking stools – you can counteract the effects of Microscopic Colitis by increasing the number of soluble fibers in your diet with foods such as oats, beans, sweet potato, avocado, and Gut Love (PHGG).
- Restoring your gut barrier function – adding or increasing pre and probiotics into your diet and restoring vitamin D levels when low can improve your gut barrier.
- Maintaining gut barrier function – increasing intake of prebiotics and plants.
What to eat if you have Microscopic Colitis
Eliminating Inflammatory Food Patterns
One of the most effective ways to reduce the number of flare-ups is to focus on adding in a more diverse diet while reducing inflammatory food patterns.
In 2020, research came out about IBD & food patterns that tended to be more inflammatory. This was consistent with what we already knew about how our microbiome is impacted by dietary patterns.
Inflammatory Food Patterns to Reduce for Microscopic Colitis are:
- Red Meats & Processed Meats (bacon, sausage, hot dogs etc)
- Myristic Acid & High Saturated Fats – Coconut oil, Palm Oil & Dairy Fats
- Gluten if you have Celiac Disease (50% of microscopic colitis patients do!)
- Certain Fillers – Carrageenan, Polysorbate 80, Carboxymethylcellulose
- Alcohol
- Artificial sweeteners
Foods to Eat with Microscopic Colitis
Knowing what you CAN eat is just as essential as knowing what to avoid so that you can plan ahead if you are grocery shopping or eating out.
Adding prebiotics, fiber, and diversity to the diet will help to reduce the risk of flare-ups. We know from research that those that do not avoid fiber are 40% less likely to have flares! Hot tip: don’t forget to drink plenty of water while increasing fiber intake.
Fiber in the diet is crucial to inflammation reduction through what we eat. Different types of fiber can also help relieve diarrhea and constipation which both can occur in microscopic colitis. Try experimenting with different recipes to make consumption more varied and enjoyable.
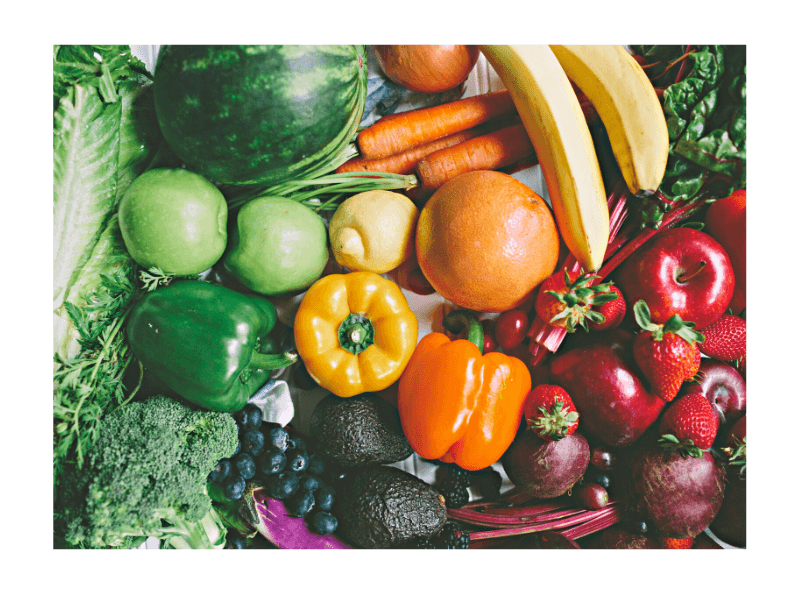
Focus on a Diverse diet:
A diverse diet, high in anti inflammatory foods can help support your immune system.
- Greens – Leafy greens like spinach, swiss chard, kale, and arugula can be a rich source of folate and phenols. Try blending, sauteing and massaging to help with tolerance.
- Berries – Berries like strawberries, blackberries, blueberries, and raspberries are rich in antioxidants which can help “clean up” the damage of having IBD and can help support some of the gut bacteria commonly low in IBD.
- Legumes – Bringing in legumes like edamame, tofu, black beans, and garbanzo beans (and many others can be helpful in creating more butyrate in the gut for inflammation reduction. If you don’t tolerate them well, try them mashed, and most importantly adopt our motto with fibers- Go low and go slow!
- Green Banana & Oat Bran – Green banana is rich in resistant starch which can help slow down transit through the digestive tract. If you’ve got diarrhea- this could help! Oats or oat bran have also been shown in studies to be great at supporting colonic butyrate production which is necessary for inflammation reduction and gut barrier healing. We encourage gluten-free oats since celiac rates are so high in microscopic colitis.
Foods Rich in Prebiotics:
- Resistant Starch – green bananas, cooked and cooled beans and potatoes.
- Colorful pigments in fruits and vegetables.
- Green tea or Matcha – still contains caffeine yet less than black tea.
- Almonds – rich in nutrients such as magnesium, vitamin E, and dietary fiber. They also make nutritious and filling snacks.
- Cacao – the seed from which cocoa and chocolate are made, a brilliant alternative to chocolate!
- Garlic – packed full of health benefits such as lowering blood pressure and cholesterol levels, boosting immunity, and reducing the length of illness.
Is Microscopic Colitis a Disability?
IBD is a disability. However, if you are looking for disability assistance or coverage, it is always best to discuss this with your insurance company. A diagnosis from a medical professional is required when being assessed for coverage.
If you are finding it difficult to work with your Microscopic Colitis diagnosis, you may qualify for a tax credit or other benefit.
Let IBD Dietitians help you to manage your Microscopic Colitis
The most important step to take if you suffer from Microscopic Colitis is to remember progress isn’t linear! Medications and nutrition changes can take time- and even if it doesn’t feel like it’s working- it doesn’t mean it isn’t.
However, also know that you do not need to do this alone. Having guidance and handing over the stress of managing your own nutrition could be just what you need.
We have tons of resources available to you at all different price points. It would be an honor to support you on your IBD journey.
At Crohn’s and Colitis Dietitians, our professional IBD specialized dietitians can guide you on your journey so you can have fewer symptoms and more confidence with your nutrition. For more information and advice contact us today and let’s get started.
References:
- Bohr, J., Wickbom, A., Hegedus, A., Nyhlin, N., Hultgren Hörnquist, E., & Tysk, C. (2014). Diagnosis and management of microscopic colitis: Current perspectives. Clinical and Experimental Gastroenterology, 7, 273–284. https://doi.org/10.2147/CEG.S63905
- Green, Peter H. R., Jun Yang, Jianfeng Cheng, Anne R. Lee, Jason W. Harper, and Govind Bhagat. “An Association between Microscopic Colitis and Celiac Disease.” Clinical Gastroenterology and Hepatology: The Official Clinical Practice Journal of the American Gastroenterological Association 7, no. 11 (November 2009): 1210–16. https://doi.org/10.1016/j.cgh.2009.07.011.
- Shor, J., Churrango, G., Hosseini, N., & Marshall, C. (2019). Management of microscopic colitis: Challenges and solutions. Clinical and Experimental Gastroenterology, 12, 111–120. https://doi.org/10.2147/CEG.S165047
- Townsend, T., Campbell, F., O’Toole, P., & Probert, C. (2019). Microscopic colitis: Diagnosis and management. Frontline Gastroenterology, 10(4), 388–393. https://doi.org/10.1136/flgastro-2018-101040
- Van Hemert, S., Skonieczna-Żydecka, K., Loniewski, I., Szredzki, P., & Marlicz, W. (2018). Microscopic colitis—Microbiome, barrier function and associated diseases. Annals of Translational Medicine, 6(3), 39. https://doi.org/10.21037/atm.2017.03.83



I am celiac, I do also have microscopic colitis and lactose intolerance. However, the doctor told me years ago he found the MC but never said change diet for it. I was given Asacol for it. It just hit me last night that maybe I should change diet as well. With having these 3 issues, I am confused as to what I can eat as some of the things I read that say I can have for one is not good for my other issue..?
Hi Laura, totally understandable. We do have resources on this topic I can share although it might also beneficial to work with an IBD focused dietitian if you are able to. We are here for you if you’d like to work on this!
Would appreciate having a complete list of foods I can truly eat with microscopic colitis. Have read so many that are confusing and contradictory. I’m on medication but seen to have way to many flare ups. Anxious to hear what you gave to say, many many thanks.
Hi Reda, I’d love to help. We have a free workshop we did on this a while back- I’ll put the link below. However, you may be looking for more than just what to eat. It sounds to me like you are looking for a plan to help with symptom reduction. Medication doesn’t always address symptoms completely- but we help many with symptom reduction. Reach out if you’d like to work with us on that!
https://www.youtube.com/watch?v=-BnI2XZ0l04&t=173s
I have several autoimmune dx including MC but find earring leafy green cause more urgency . Lord knows I have enough hard time getting to the bathroom wo an accident
Understandable. This information is really meant to be a starting point – to help share more of the research that’s available to us. But when we work 1:1 with clients – we work on specific strategies to help reduce symptoms like urgency… but it’s certainly hard to get that sort of nutritional guidance from a blog. If you’d like any support- don’t hesitate to reach out!
I have been suffering with MC diagnosed via biopsy after a colonoscopy 2 years ago. Yours are the first first recommendations that sound credible. Kept telling me BRAT type diet. Found fiber was helpful, and stopped by morning coffee replacing it with Matcha Tea. Juggling between flares of watery diarrhea, followed by constipation as the diarrhea recedes. Maddening! Thank You for your information .
That’s refreshing to hear that you are finding our writing helpful! I’m so glad…
‘m totally confused. One article says no fat, no dairy, and no fiber, or lequemes, and this site says to eat all those!!!!!
And the doctor didn’t recommend any diet changes.
I totally get it. With everything on the internet it can be hard to know who to trust. We did a free deep dive on the topic – I’ll put a link below. I’m sorry to hear your doctor didn’t suggest any nutrition support – there is a lot of research showing how helpful it can be! I’d be happy to chat with you personally too. Check out the video first though! It might help connect the dots.
https://www.youtube.com/watch?v=-BnI2XZ0l04&t=173s
I have suffered from what appears to be MC since the weeks long attack started on Oct. 23. I won’t get a colonoscopy till Dec. 8, but I like your food recommendations. Any more colorful fruit suggestions? Are you saying that spinach and other leafy greens need to be cooked first? And white potatoes? Really? I heard that they were bad. I have really suffered. Please advise.
I’m sorry to hear you’ve been suffering- and glad we could help. As far as color- getting as much variety as possible is good. Cooking and blending can help improve tolerance and help reduce symptoms. Yes, as far as research on this goes- getting more color and plants in the diet can help reduce risk of flare and it is associated with lower fecal calprotectin (a marker of inflammation). White potatoes are actually a rich source of minerals and antioxidants believe it or not- also to amplify the benefits you can cook and cool them before eating which increases the resistant starches in them!
I would like my daughter to have an interview with you. How does this happen?
I’d be happy to chat! Here is a link to schedule with a free chat: https://p.bttr.to/3wTGxab