Inflammatory bowel disease (IBD) is a common chronic condition that impacts the lives of millions around the world. Crohn’s Disease and Ulcerative Colitis are the two most common types of IBD.
With its prevalence on the rise, understanding the role of gut health in managing IBD is crucial. In this blog, we will delve into the evidence behind probiotics for IBD. We will also answer the question, which probiotics help for IBD?
From discussing probiotic products for Crohn’s Disease, Ulcerative Colitis, Microscopic Colitis, and Pouchitis, symptom control, and the essential strain specific approach, this blog aims to equip you with the knowledge needed to navigate the complexities of IBD and improve the health of your gut.
Probiotics are a hot topic in the gut space. In my experience though, I feel most people are using them the wrong way and just taking any strain with hopes that it will help. If you are hoping that a probiotic will help with bloating for example, make sure the strain you are using has evidence to do just that!
I hope this blog will help provide some clarity on a misunderstood topic. Remember, as always, this is not medical advice. Chat with your IBD dietitian and gastroenterologist about if probiotics are a good option for you. If you need an IBD dietitian, let’s chat.
The Evidence for Probiotics in IBD
In the last blog I discussed probiotic use for people with IBD. There are three considerations to consider before purchasing a probiotic. If you haven’t already- check it out. Also, it will help break down the reasons why this topic can be so polarizing.
In this blog, I’ll provide an overview of some (but definitely not all) of the research on probiotics in IBD.
In our practice, there are many considerations we have before advising on which probiotic is best for someone to help with IBD and their overall health. So, be sure to check in with your health care team and IBD dietitian. In addition, you have to get guidance on how to best use this information.
Which Probiotics Help for IBD?
Probiotics for UC
There are a variety of probiotics that can be used to help induce remission and reduce symptoms in UC patients. We have narrowed the list down to our most commonly recommended probiotics below.
Visbiome
A Meta-analysis found Visbiome (formerly VSL #3) to be effective in inducing remission in active ulcerative colitis. It was found that Visbiome may be effective in inducing remission in active UC. Visbiome probiotics in this meta-analysis study were found to be as effective in preventing a relapse of UC as 5 Aminosacylates– the common drugs used to treat IBD. [1]
*If you’d like a discounted version of visbiome, you can set up a free account on our fullscript HERE.
Lactobacillus Rhamnosus GG
The LGG strain was found to be equally effective as mesalamine in maintaining clinical remission. It is significantly more effective than mesalamine in prolonging the relapse-free time. [17]
Back to Balance Plus, L.plantarum 299v
Back to Balance plus is one of our top recommendations. Its use with both UC and IBS symptom reduction (see below). In mild to moderate Ulcerative Colitis patients the L.plantarum 299v strain in a drink form has also shown some use with helping to reduce symptoms like bloating, stool frequency, abdominal pain and helping to induce remission [8]. Also, the L.plantarum 299v strain can help with reducing antibiotic associated diarrhea, and reduce risk of C.diff infection in critically ill patients [7].
Microscopic Colitis
Can We Help? Get in Touch:
For those of you less familiar with this type of colitis- microscopic colitis is a less common type of inflammatory bowel disease that affects the large intestine. The two types of microscopic colitis are lymphocytic and collagenous colitis.
The most common symptom is persistent watery diarrhea. Microscopic colitis got its name from the fact that tissue typically appears normal in a colonoscopy and requires a microscope to diagnose.
I’ve listed two strain combinations that we know of so far that have evidence for microscopic colitis.
Lactobacillus acidophilus La5 and Bifidobacterium lactis Bb12
In a study looking at using probiotic strains Lactobacillus acidophilus La5 and Bifidobacterium lactis Bb12- compared to baseline- there was a reduction in weekly bowel frequency and a reduction in number of days with liquid stools per week- from 6 to only 1. [16]
There are a few brands that carry this strain, however some of them also contained chicory root and things that could cause additional symptoms. Trubiotics was the only one I’ve found so far without additional ingredients, you can find it HERE.
Visbiome
Patients with active microscopic colitis who received Visbiome (VSL#3) at a dose of 900 billion CFU’s when compared to patients receiving mesalamine at 1.6 g/day, had a clinical remission rate of 46% of patients compared to 8% in the mesalamine group, and less stool mucus after 8 weeks of supplementation. [12]
*If you’d like a discounted version of visbiome, you can set up a free account on our fullscript HERE.
Probiotics for Crohn’s
With Crohn’s Disease there are less options for evidence based probiotics than with Ulcerative Colitis. In fact, there are studies showing negative results with strains Lactobacillus rhamnosus GG and Lactobacillus johnsonii LAI for Crohn’s Disease patients (13, 11).
In our practice we take a variety of different approaches for people with Crohn’s when it comes to evaluating which supplementation will yield the best and fastest results. Oftentimes, rather than probiotics, we use prebiotics to reduce symptoms in treating Crohn’s Disease.
If there are more IBS symptoms present we might also consider using a probiotic with evidence for reducing symptoms. When it comes to reducing Crohn’s activity and symptoms specifically, there is only one strain to date with evidence.
Check out our most recent video on prebiotics which is also at the bottom of this article.
Saccharomyces Cerevisiae Boulardii Bicodex
In CD patients with mild-moderate activity, co-administration of this strain supplemented led to a significant reduction in stool frequency and improvements in CDAI index (8). In combination with mesalamine, using the probiotic bacteria of biocodex strain led to reduced relapse rate compared to mesalamine alone- 6% vs 38% (link).
It’s important to also acknowledge that there have been some studies that show some reaction to saccharomyces cerevisiae, but this is not true for the biocodex strain. FloraStor is the only brand of probiotic currently that I’m aware of that carries this strain.
Pouchitis
Pouchitis can occur after surgery to treat ulcerative colitis or certain other diseases. Moreover, many people with ulcerative colitis need to have their colon removed and the bowel reconnected with a procedure called J-pouch surgery.
Pouchitis is inflammation that occurs in the lining of a pouch created during surgery to treat ulcerative colitis or certain other diseases. Although it’s not an extensive list, there are a few strains of probiotics that can be both helpful in the treatment and prevention of pouchitis.
Visbiome
In patients who underwent surgery for ulcerative colitis, 1-year supplementation with Visbiome (VSL#3) at 900 billion CFU’s a day immediately after ileostomy closure, significantly reduced episodes of acute pouchitis and improved quality of life. [5]
In those patients that already had pouchitis and were treated with Visbiome. Also, 69% of subjects achieved remission after treatment; significant reductions in mean pouchitis disease activity index scores from baseline [6]
*If you’d like a discounted version of visbiome, you can set up a free account on our fullscript HERE.
Lactobacillus Rhamnosus GG
Significantly delayed first onset of pouchitis compared to no-treatment controls. The risk for pouchitis increases by year 3. While those on the LGG strain were able to prolong the onset up to 7 years. [7]
The LGG strain is commonly found in Culturelle. If you use our link here – you’ll get a discount on it as well once you sign up for a free account.
Probiotics for IBS
Approximately, half of those with Inflammatory Bowel Disease also have IBS or irritation symptoms despite being in clinical remission without inflammation [15]. In addition, compared to the general population, those of us with IBD have a three fold greater chance of having IBS symptoms [15].
While inflammation reduction and reduced risk of flare is the priority for IBD patients, helping support symptom reduction can greatly improve quality of life. There are many probiotics I wanted to include here for IBS- both food based and supplement versions.
To keep things brief- I kept the list to my all time favorite strain that we have seen the most positive results in using.
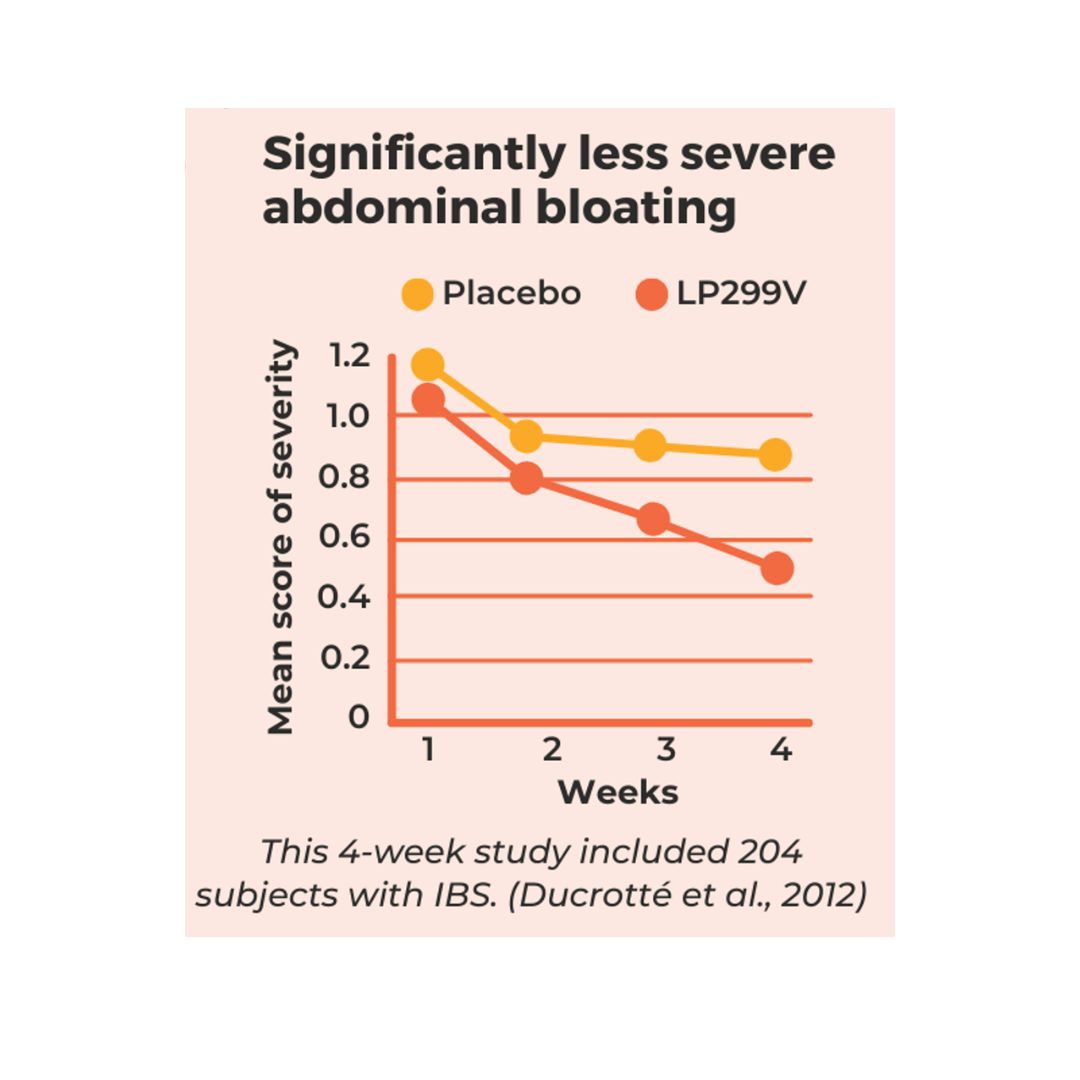
Lactobacillus Plantarum 299V
Studies on L. plantarum 299v have established it as a probiotic for IBS symptoms based on the 2017 guidelines of the World Gastroenterology Organisation.
Back to Balance Plus is my most commonly used probiotic supplement because it’s one I’ve had the highest success rate with for those that suffer with painful abdominal pain and bloating [4]. Moreover, the strain found in Back to Balance plus was shown in a 4 week treatment period to reduce painful IBS symptoms like bloating and abdominal pain in 78% of the individuals that took it [4].
Probiotics, Mental Health & IBD
Often when we discuss IBD symptoms, we only talk about gut symptoms. However, many IBD patients also deal with depression, anxiety and medical trauma. This can significantly impact quality of life and even impact our ability to recover and respond to treatment interventions.
While I’ll be covering this in more depth in my next post, I did want to call out two probiotic strains with promising early evidence to support mental health especially when combined with other layers of support.
Lactobacillus helveticus R0052 & Bifidobacterium longum R0175
In a randomized, placebo controlled human study of 55 volunteers (age- 33-60) with mild depression or anxiety, some took a placebo while others took a mixture of 3 billion CFU’s of the probiotic and they found [3]:
- 50% improvement in depression scores
- 36% improvement in hospital anxiety and depression scale
- 49% improvement in global severity index (measures stress)
- 60% improvement in anger-hostility scores
- 13% decrease in urinary cortisol (measure of stress)
- Improvements also in self blame and problem solving
- Three weeks after, probiotic group had 7.6 times the reduction in abdominal pain compared to placebo. Also, there was 2.1 times less stress induced nausea and vomiting, 2.9 times less gas and bloating
This probiotic and all others listed on this blog can be found in our favorites list on fullscript.
A Final Note on Probiotics
You might be wondering- how do you know if probiotics are working? It isn’t easy to determine this based on symptoms alone. As I’ve mentioned in other articles on the types of remission, symptoms alone aren’t always the best indicator of inflammation and our IBD.
We can be symptom free and have ongoing disease activity and inflammation. Also, we can also have irritation symptoms like gas, bloating, diarrhea (etc) and have no inflammation present. Not to mention, side effects that may occur from certain IBD medications.
The research which probiotics help for IBD can vary quite a bit on how long it takes to see results. Some studies showing symptoms improving 6 months to a year after taking probiotics.
It’s important to realize that most of the time it’s not one thing that makes a difference for IBD. So, it’s a layered approach of bringing in many evidence based strategies with probiotics having the potential to be one of them.
If you are looking for more great reads like this one- Check out our new blog on our most requested topic – Probiotics for Bloating.
Looking for help on symptom relief? Start here
Symptoms like bloating, abdominal pain, diarrhea and constipation can turn your world upside down with IBD. Did you know that even when inflammation and disease activity are managed well – you can still have symptoms with IBD?
This can make trying new foods a bit scary for many people. You might not even know where to start. If this is you, let us help! Work with us 1:1 and get:
- Get a customized plan in place for your IBD
- Expand your diet without triggering symptoms
- Reduce your risk of flare-ups long-term
- Improve energy so you can get back to what you enjoy
- Get clear on what matters the most – so you can let go of what doesn’t matter as much
If that sounds like what you are looking for- join us! When you work with us, we are with you every step of the way and we offer more support and resources than you could dream of.
Resources:
- AC; Derwa Y; Gracie DJ; Hamlin PJ; Ford. “Systematic Review with Meta-Analysis: The Efficacy of Probiotics in Inflammatory Bowel Disease.” Alimentary Pharmacology & Therapeutics, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/28653751/.
- “Aminosalicylates.” Crohn’s & Colitis Foundation, https://www.crohnscolitisfoundation.org/what-is-ibd/medication/aminosalicylates.
- Chao, Limin, et al. “Effects of Probiotics on Depressive or Anxiety Variables in Healthy Participants under Stress Conditions or with a Depressive or Anxiety Diagnosis: A Meta-Analysis of Randomized Controlled Trials.” Frontiers in Neurology, Frontiers Media S.A., 22 May 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7257376/.
- Ducrotté, Philippe, et al. “Clinical Trial: Lactobacillus Plantarum 299V (DSM 9843) Improves Symptoms of Irritable Bowel Syndrome.” World Journal of Gastroenterology, Baishideng Publishing Group Co., Limited, 14 Aug. 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3419998/.
- Gionchetti P; Rizzello F; Helwig U; Venturi A; Lammers KM; Brigidi P; Vitali B; Poggioli G; Miglioli M; Campieri M; “Prophylaxis of Pouchitis Onset with Probiotic Therapy: A Double-Blind, Placebo-Controlled Trial.” Gastroenterology, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/12730861/.
- Gionchetti P; Rizzello F; Morselli C; Poggioli G; Tambasco R; Calabrese C; Brigidi P; Vitali B;Straforini G; Campieri M; “High-Dose Probiotics for the Treatment of Active Pouchitis.” Diseases of the Colon and Rectum, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/17934776/.
- Gosselink MP; Schouten WR; van Lieshout LM; Hop WC; Laman JD; Ruseler-van Embden JG; “Delay of the First Onset of Pouchitis by Oral Intake of the Probiotic Strain Lactobacillus Rhamnosus GG.” Diseases of the Colon and Rectum, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/15108026/.
- J, Plein K; Hotz. “Therapeutic Effects of Saccharomyces Boulardii on Mild Residual Symptoms in a Stable Phase of Crohn’s Disease with Special Respect to Chronic Diarrhea–a Pilot Study.” Zeitschrift Fur Gastroenterologie, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/8465554/.
- Klarin B; Wullt M; Palmquist I; Molin G; Larsson A; Jeppsson B; “Lactobacillus Plantarum 299V Reduces Colonisation of Clostridium Difficile in Critically Ill Patients Treated with Antibiotics.” Acta Anaesthesiologica Scandinavica, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/18840110/.
- Krag A; Munkholm P; Israelsen H;von Ryberg B; Andersen KK;Bendtsen F; “Profermin Is Efficacious in Patients with Active Ulcerative Colitis–a Randomized Controlled Trial.” Inflammatory Bowel Diseases, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/24108114/.
- Marteau P; Lémann M;Seksik P; Laharie D; Colombel JF; Bouhnik Y; Cadiot G;Soulé JC;Bourreille A;Metman E;Lerebours E; Carbonnel F; Dupas JL;Veyrac M;Coffin B;Moreau J;Abitbol V;Blum-Sperisen S;Mary JY; “Ineffectiveness of Lactobacillus Johnsonii LA1 for Prophylaxis of Postoperative Recurrence in Crohn’s Disease: A Randomised, Double Blind, Placebo Controlled GETAID Trial.” Gut, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/16377775/.
- Rohatgi, Sarika, et al. “VSL#3 Induces and Maintains Short-Term Clinical Response in Patients with Active Microscopic Colitis: A Two-Phase Randomised Clinical Trial.” BMJ Open Gastroenterology, BMJ Publishing Group, 9 Feb. 2015, https://www.ncbi.nlm.nih.gov/pubmed/26462271.
- Schultz, Michael, et al. “Lactobacillus GG in Inducing and Maintaining Remission of Crohn’s Disease.” BMC Gastroenterology, BioMed Central, 15 Mar. 2004, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC394324/.
- Simrén M; Axelsson J; Gillberg R; Abrahamsson H;Svedlund J;Björnsson ES; “Quality of Life in Inflammatory Bowel Disease in Remission: The Impact of IBS-like Symptoms and Associated Psychological Factors.” The American Journal of Gastroenterology, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/11866278/.
- Simrén M;Axelsson J;Gillberg R;Abrahamsson H;Svedlund J;Björnsson ES; “Quality of Life in Inflammatory Bowel Disease in Remission: The Impact of IBS-like Symptoms and Associated Psychological Factors.” The American Journal of Gastroenterology, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/11866278/.
- Wildt, Signe, et al. “Probiotic Treatment of Collagenous Colitis: A Randomized, Double-Blind, Placebo-Controlled Trial with Lactobacillus Acidophilus and Bifidobacterium Animalis Subsp.. Lactis.” Inflammatory Bowel Diseases, U.S. National Library of Medicine, May 2006, https://www.ncbi.nlm.nih.gov/pubmed/16670529.
- Zocco MA;dal Verme LZ;Cremonini F;Piscaglia AC;Nista EC;Candelli M;Novi M;Rigante D;Cazzato IA;Ojetti V;Armuzzi A;Gasbarrini G;Gasbarrini A; “Efficacy of Lactobacillus GG in Maintaining Remission of Ulcerative Colitis.” Alimentary Pharmacology & Therapeutics, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/16696804/.












Can / should probiotics be taken during a flare?
Hi Kelly! There is research on certain strains being effective at inducing remission during IBD flares. There is also research on certain strains for reducing bloating, urgency and bowel frequency. It’s about matching the right strain with your top priority! Let us know if you need help with that, we would be happy to consult with you. You can schedule a call with us below if needed.
Schedule a Inquiry call to Work with us ⬇️
https://p.bttr.to/2VpevRX
“If there are more IBS symptoms present we might also consider using a probiotic with evidence for reducing symptoms. When it comes to reducing Crohn’s activity and symptoms specifically, there is only one strain to date with evidence.”
Hi, you said this, but what is the strain called please?
For Crohn’s we prefer prebiotics over probiotics.
The only one with some research for Crohn’s is below. But they have many varieties now (some with other stuff that can trigger symptoms) – so I’ll put a direct link:
https://amzn.to/3NVO8k5
Great breakdown of how different probiotic strains can support IBD management! It’s so important to understand which strains are effective rather than taking a one-size-fits-all approach. Worth a read if you’re navigating gut issues or supporting someone who is.