Four Myths about IBD
It can be tricky to see through common myths and find the right advice when diagnosed with IBD, and this is something our team knows first-hand.
Our Registered Dietitians specialize in providing nutritional support and guidance to those living with Inflammatory Bowel Diseases: Crohn’s and Colitis.
Not only are we a team of 4 dietitians that specialize in IBD, but we also have IBD. While each of us have a background in nutrition, we felt at a loss when it came to finding reliable IBD support and education.
Misconceptions about IBD are common
Several myths and misconceptions about IBD are perpetuated both online and within the healthcare system.
This can be misleading, frustrating, and confusing – not what you want when looking for health advice! Myths about Inflammatory Bowel Diseases are often born out of anecdotal evidence, rather than science, and from outdated beliefs.
The combination of our professional expertise and personal experience of IBD grants us a unique perspective when challenging misconceptions and helping our clients.
We can advise on and discuss Crohn’s and Colitis using a valuable combination of our personal and professional standpoints. And we truly understand how universal our IBD experiences are.
Part of this universal experience is, unfortunately, trying to identify truth amongst myths.
The internet means misconceptions about IBD are pretty impossible to avoid. That’s why we’ll be discussing a selection of common myths about Crohn’s and Colitis in this blog, using our experience and nutrition background to give you the reliable advice that you deserve.
Read on below…
Myth #1 – Stress can cause IBD
Years ago, it was believed by healthcare professionals that IBD was partially caused by psychological issues, such as stress.
Although this belief has now been disproved, it can take a long time for misconceptions to disappear from everyday conversations and unsolicited advice on the internet.
We know now that IBD is not caused by stress in the first place. But we can say with confidence, that prolonged stress triples your risk of a flare-up.
The bottom line is that stress is bad for our health, and IBD is not an exception to this rule. Whether it causes a flare-up or makes your everyday symptoms worse, we know from both a personal and professional perspective that stress can impact Crohn’s and colitis.
If you’re currently on an IBD treatment plan but feel it’s not working as well as it should, we urge you to consider all the variables, including your personal lifestyle and mental health.
Myth #2 – It’s impossible to treat IBD
Inflammatory Bowel Disease is a chronic condition, but that doesn’t mean it can’t be treated.
There is no definitive cure for either ulcerative colitis or Crohn’s disease at this moment in time, but there are treatments available that can lessen your symptoms.
Treatment ranges from medicines that reduce inflammation or the response of the immune system and surgery for those with severe symptoms, to diet and lifestyle therapy that’s totally tailored to you. You may well need to work with an IBD specialist to get the right kind of treatment and nutritional therapy.
As Registered Dietitians who are dedicated to working with fellow IBD sufferers, our main goal is to get our clients into symptom remission and stay there for as long as possible. And we know from personal and professional experience that this can be done.
Myth #3 – Your diet doesn’t impact your IBD symptoms
Following on nicely from the last myth, let’s talk about the misconception that what you eat doesn’t affect IBD.
Similar to medication, what you eat cannot cure your IBD forever, and your diet is certainly not the only thing that impacts symptoms. Having said that, it’s misleading to say that nutrition has no role to play.
Doctors who tell their IBD patients that their diet makes no difference to their health or symptoms are ignoring contemporary evidence. For example, we know that eating fast food several times a week can lead to a huge 390% increased risk of an IBD flare-up.
The fact is that different diet styles affect our gut microbiome differently, and this means that some diets are more likely to lead to flare up, while others improve the health of your gut and support remission.
Plus, it’s vital to remember that nutrition isn’t solely about what you eat. It also involves looking for and treating deficiencies and intolerances that can most certainly be a barrier to remission.
Suggesting that diet has no role to play in IBD can devalue the importance of nutrition in IBD management and means that countless sufferers get less effective treatment.
If your doctor has belittled the importance of diet in your treatment plan, remember that you know your personal symptoms and triggers best. As Registered Dietitians, we know that IBD patients themselves are well aware that diet and nutrition have an impact.
Myth #4 – IBD is the same as IBS
This is an IBD misconception that causes frustration for many.
Inflammatory bowel disease and irritable bowel syndrome are two very different conditions. Symptoms may cross over and diet can impact both, but that’s where the similarities end.
Crohn’s and colitis, the most common types of IBD, both cause chronic inflammation of the GI tract. They can lead to serious damage which can increase your risk of colon cancer.
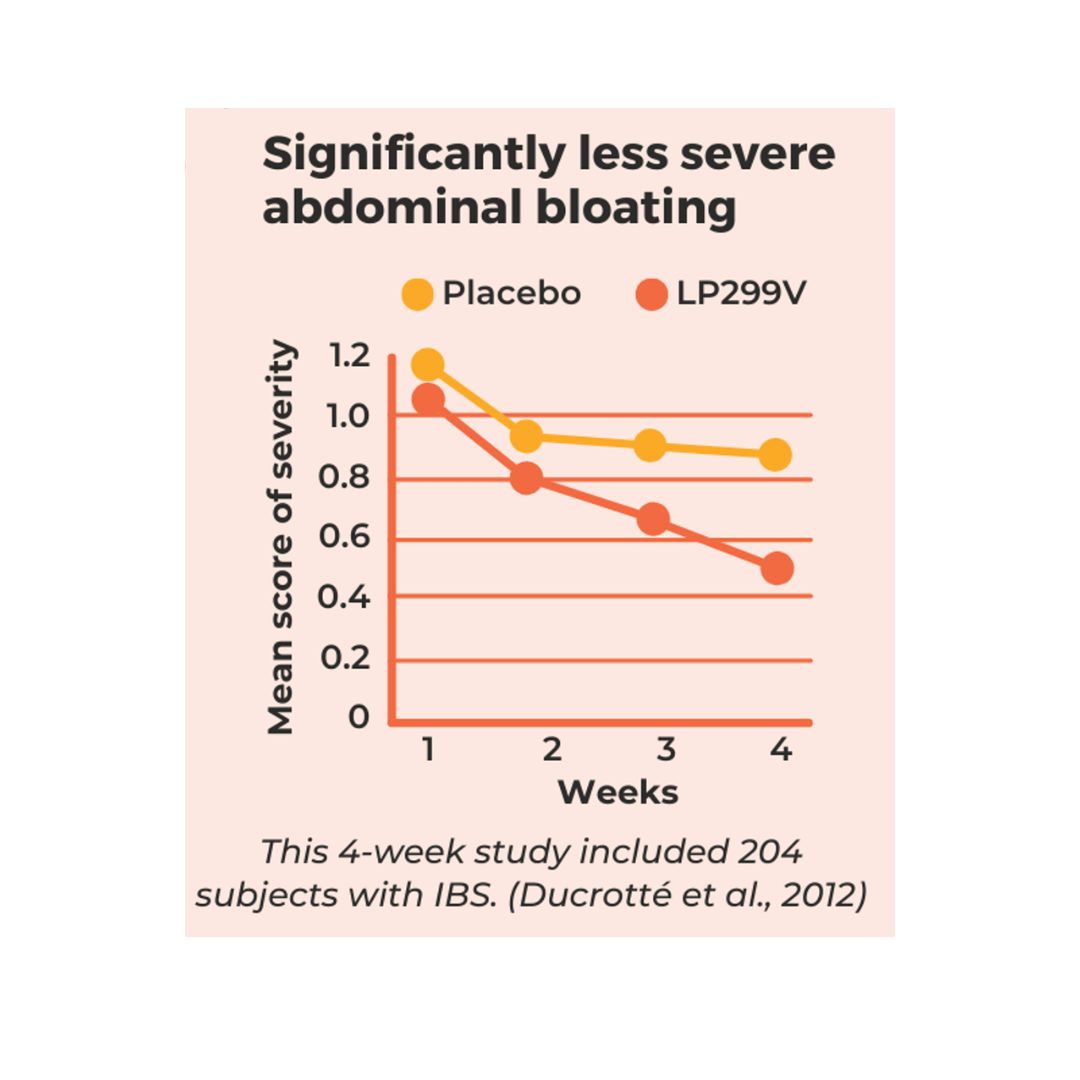
IBS can cause unpleasant symptoms and emotional distress, but it doesn’t lead to inflammation or damage to the digestive system. Medication and surgery are usually not needed to treat patients with IBS, as flare-ups can largely be managed successfully by simply recognizing and minimizing an individual’s triggers.
So while we would never dismiss IBS as an easy condition to live with, it is fundamentally different from IBD. Confusing the two can mean IBD sufferers are not treated fairly by employers, for example.
Get the IBD help you need and deserve
We hope this post provided a candid and refreshing look at common myths about IBD, and perhaps even provided you with validation if you feel brushed off by doctors or peers.
There are treatment opportunities available for all with IBD, and our Crohn’s and colitis dietitians can help you get the nutritional support that you deserve. We have several options – both for those ready to get started with a solidified plan and for those just looking to learn!
Give your gut some love and get started today.



YES very different! Thank you for making me aware of the mistake…. I had someone edit the post for me and I guess they mixed that part up. Kind of ironic that the blog highlights the differences too! Funny…
IBD is Inflammatory Bowel Disease not Irritable… big difference