Probiotics for Crohn’s Disease
There’s a lot we don’t know about Crohn’s disease, including what causes the disease and how to cure it. However, probiotics are a promising area of study, and it already has good initial results with other types of inflammatory bowel disease (IBD), such as ulcerative colitis.
In Crohn’s disease, all or parts of the bowels (large and small intestine) are inflamed due to an overactive immune response. Studies have linked Crohn’s disease to lower diversity in the gut microbiome, the community of bacteria that resides in our guts.
A lot of people, including experts, are proposing that probiotic foods and supplements are treatments for Crohn’s disease, but are they right? Let’s explore the research and evidence for these claims.
What are probiotics?
Probiotics are a mixture of live, helpful microorganisms such as yeast and bacteria that are beneficial to us as the host when we consume them.
The human gut has a microbiome of trillions made up of bacteria, fungi, and various microbes, the majority of which lives in the intestines.
Some of these organisms are “good” while others can be nasty, which is why a balanced microbiome is critical. The microbiome is critical for the digestion and absorption of food, produces some vitamins, and plays a critical role in our immune system. Hence, a healthy microbiome is essential for good health.
Ideally, your gut microbiome should be highly diverse, with 300-500 strains of bacteria among other microbes. Fewer strains or a lower population causes an imbalance, which can contribute to other problems such as irritable bowel syndrome, diarrhea, and even immune system issues.
Taking live bacteria in probiotics or probiotic foods can be a helpful way of restoring the numbers and diversity of the gut microbiome.
Probiotics are essentially capsules full of live bacteria that you take to add to your gut microbiome.
You may also have heard about prebiotics, which are compounds and foods that help feed and maintain the bacteria in your gut. Probiotics seem to absorb better when taken with prebiotic-rich foods like onions, garlic, and green tea.
Why all the confusion about probiotics in IBD?
Several clinical trials have been carried out to investigate the use and benefits of using probiotics to maintain remission in IBD. So far, the results have been inconsistent as a whole, mostly because there are so many factors involved.
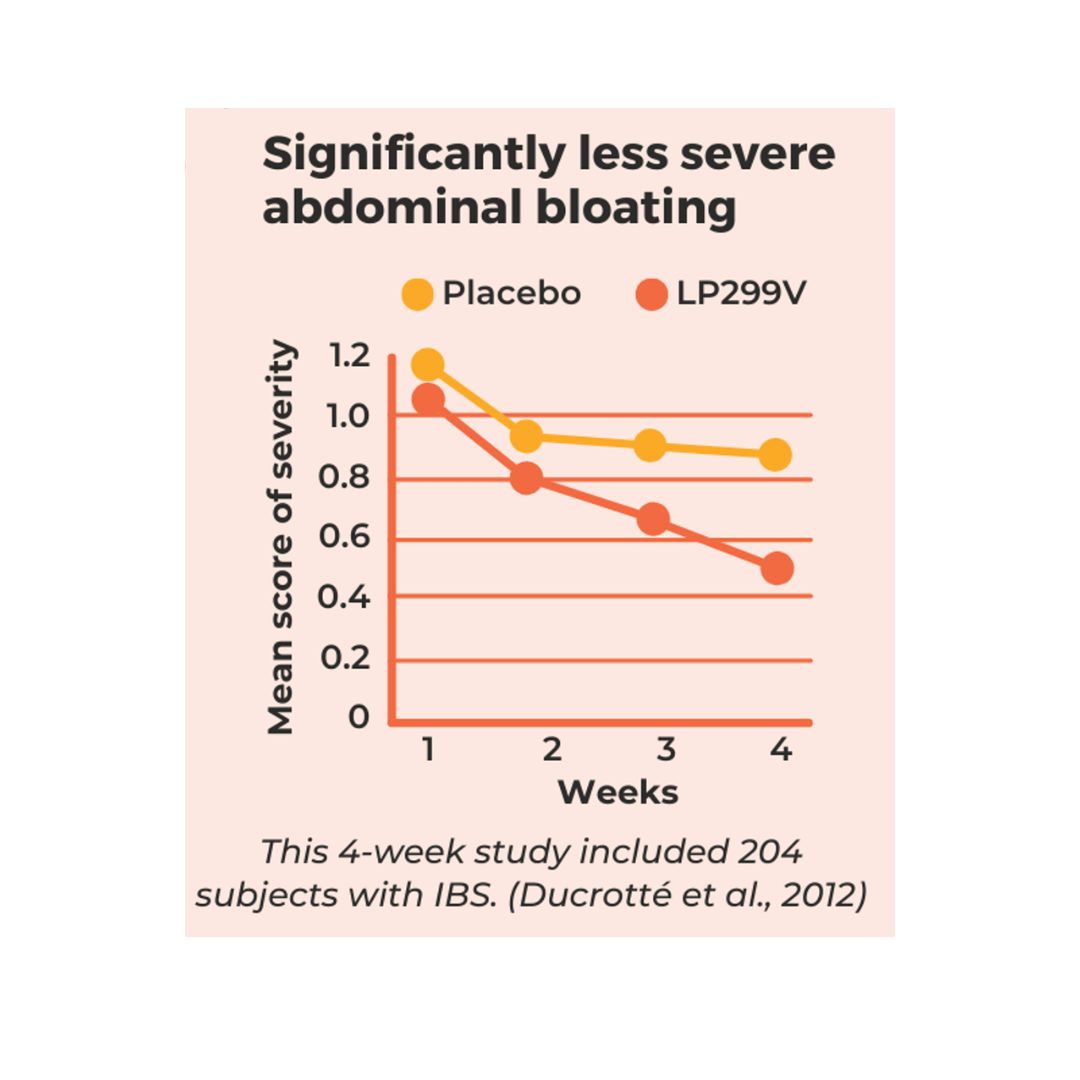
Most of the quality research is around ulcerative colitis, microscopic colitis and IBS, which affects up to half of IBD patients. In one review of over 60 studies relating to probiotics and IBD, researchers concluded that more evidence supported the use or probiotics for the treatment of ulcerative colitis (UC) rather than Crohn’s disease.
In their book New Insights into Inflammatory Bowel Disease, researchers Karen Kroeker and Cathy Lu concluded that “there is insufficient evidence to support the use of probiotics in the management of Crohn’s disease at this time.”
On the other hand, there are some smaller studies that point towards probiotics and their effectiveness in treating the symptoms of Crohn’s disease and encouraging longer remission. Why all this confusion?
One of the reasons could be that the effect of probiotics varies between hosts. IBD is a complex disease with many resulting from the interplay of genetic and environmental factors. Both Crohn’s and Ulcerative Colitis fall under this umbrella term and are all complex and usually life long diseases.
Another factor is that probiotics affect different aspects of IBD. This makes it very difficult to say that one strain is beneficial for everyone with the same disease. There are many factors at play, including:
- Genetics
- Inflammatory changes
- Severity of disease
- Environment
- Microbiota composition and changes
- Others
We suggest using a “strain-specific” approach
We agree with researchers that larger studies are needed to help identify which strains of probiotic bacteria are helpful in treating Crohn’s and IBD in general.
Such a “strain specific approach” considers that not all strains of bacteria in a probiotic family are the same. Each strain has different effects that could work for certain symptoms and patients but not for others.
Probiotics’ anti-inflammatory effect depends on the strain type and the dose used. For this reason, we encourage a strain-specific approach to specifically target one or more symptoms that you are aiming to address.
For more information on well-researched probiotic strains for certain ailments, check out the US Probiotic Guide.
How can probiotics help with Crohn’s?
Because the gut microbiome is altered in patients with Crohn’s disease, probiotic therapy is an attractive treatment option because it helps support the microbiome and potentially alleviate symptoms of Crohn’s disease (source).
Although we don’t fully understand the mechanisms around Crohn’s disease, probiotics may help by improving the intestinal barrier and by strengthening and tightening junctions in the gut wall. The gut is the first line of defense against pathogens and is also crucial for the IBD healing and recovery process.
For now, most probiotic strains that have been shown to be helpful in IBD are more for ulcerative colitis and microscopic colitis rather than Crohn’s.
It’s important to consider the type of strain used anytime using probiotics since some strains can actually cause more harm or damage in certain cases. For example, in this case study, Lactobacillus rhamnosus GG (Culturelle) was associated with some strains that may even intensify symptoms in Crohn’s.
Probiotics with evidence for Crohn’s
There is limited research regarding the effectiveness of probiotics in treating Crohn’s disease. To date, many sources conclude that probiotics have a minimal or no effect. In fact, ESPEN guidelines for clinical nutrition suggest that probiotics in Crohn’s are not helpful at all.
It’s important to remember that probiotic research in Crohn’s, is still in its infancy. There is a lot more to learn and know about probiotics and how they interact with Crohn’s.
One study suggested evidence that Florastor (S. boulardii) improves intestinal permeability, helped maintain remission, and bowel sealing in Crohn’s.
In another study, Faecalibacterium prausnitzii showed anti-inflammatory properties in Crohn’s. However, this particular probiotic isn’t available for purchase yet.
How about probiotic-rich foods?
If you aren’t ready to start taking probiotic supplements yet, you can start with probiotic foods. These have an almost zero risk profile in treating IBD and Crohn’s disease. They can also help improve overall health.
Most probiotic foods are the fermented kind. Examples include:
- Kefir
- Kombucha
- Tempeh
- Miso
- Sauerkraut
- Kimchi
You can also take prebiotic-rich foods which help promote and feed the microbiome in your gut. These also tend to be very good for digestive health, which is important for IBD nutrition.
Prebiotic foods
Most prebiotics are dietary fibers that are hard to break down in the initial stages of digestion. This means the bacteria in your gut get to break these down and unlock the nutrients in them for their own use.
The best prebiotic foods include:
- Resistant Starch- Green Bananas, Cooked and cooled beans and potatoes
- Colorful pigments in fruits and vegetables
- Green tea
- Almonds
- Cacao
- Garlic
Some experts feel that probiotics shouldn’t be considered an option for the treatment of Crohn’s due to the lack of good quality evidence. However, the lack of large studies doesn’t mean that good quality evidence in smaller cohorts doesn’t exist.
Taking this into consideration and coupling it with what we know of prebiotics and their nourishing dietary patterns, we believe that their overall benefits in the management of IBD can be amplified.
Bottom line
Probiotic therapy should be considered on a case-by-case basis by a specialized healthcare provider.
Some probiotics could be effective in treating Crohn’s disease but may not be beneficial to you due to various factors. It’s important to weigh the pros and cons of probiotic therapy in IBD with a trusted provider that can help determine which strategy is best for you.
Book your appointment today with a Crohn’s and Colitis Dietitian and let us guide you on your way.













I have Crohn disease and is taking probiotics.Wondering if this is safe to do so ?