Inflammatory Bowel Disease (IBD) is a group of diseases that includes Ulcerative Colitis and Crohn’s Disease. IBD is a relapsing-remitting immune disorder of the gastrointestinal tract. Because IBD is an immune-mediated inflammatory disease, nutrient deficiencies are common.
Common deficiencies in IBD include:
- Iron
- Calcium
- Vitamin D
- B vitamins like B12
- Antioxidants like vitamin C, E, and Zinc
Vitamin D is an especially important nutrient in IBD and is a particularly buzzworthy topic globally right now.
The prevalence of vitamin D deficiency in IBD is 30-40%, with higher percentages in Crohn’s Disease as well as in those living in places further from the equator (19).
Overview of Inflammatory Bowel Disease
IBD is not a single disease, but a group of symptoms that can be caused by several conditions.
Crohn’s Disease
Crohn’s Disease is a type of IBD caused by chronic inflammation of the gastrointestinal tract. The causes are still not known for most patients, but genetics, the environment, and diet may be contributing factors. Adolescents and young adults are most likely to suffer from it.
Ulcerative Colitis
Ulcerative Colitis is a type of IBD that causes inflammation or ulcers of the digestive tract. As with Crohn’s Disease, symptoms vary greatly, and the symptoms of these two conditions are often very similar.
Microscopic Colitis
Microscopic colitis is a type of intestinal inflammation that is also considered an IBD. It is distinguished from other types of IBD in that it can only be detected with a microscope.
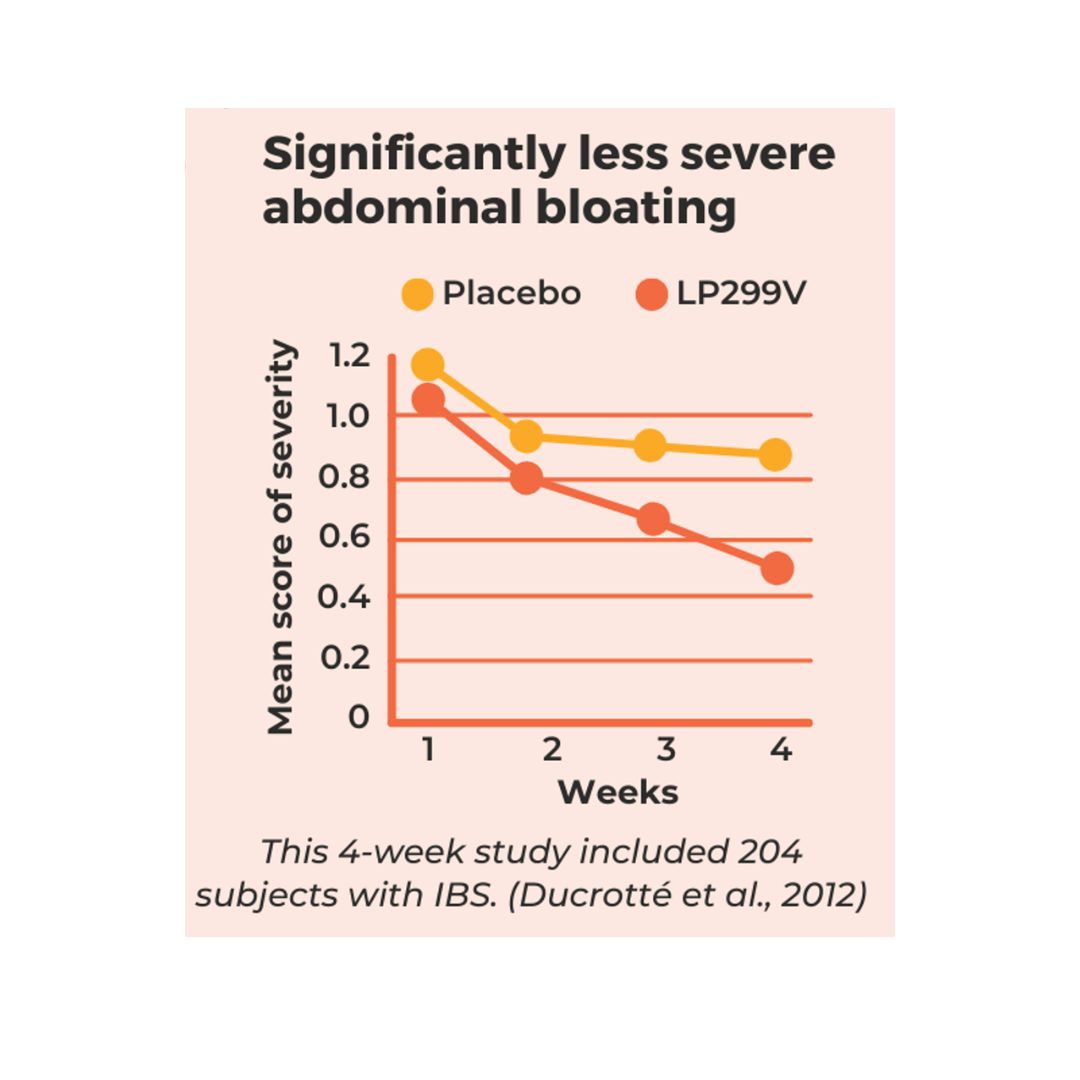
IBD vs IBS
Inflammatory bowel disease is sometimes confused with irritable bowel syndrome (IBS). Although the symptoms of the two can overlap, they are distinct. IBS is classified as a functional disorder of the gastrointestinal system, meaning that it causes symptoms in that area. IBD is more serious as it involves inflammation of the intestines and often vitamin and mineral deficiencies. It can also lead to other diseases such as colorectal cancer. While IBD and IBS are different, it’s possible to suffer from both. For more about IBD, Contact Us.
What is Vitamin D?
Vitamin D actually isn’t a vitamin at all!
Vitamin D is a family of molecules that act as a steroid hormone in the body when the skin is exposed to sunlight. Vitamin D is also synthesized in other animals and plants, which can be ingested by humans.
It’s long been established that vitamin D is extremely important for bone health, but in recent years it has been recognized as a key regulator in immune function as well, with evidence to suggest vitamin D as a regulator of gastrointestinal inflammation (17).
Because vitamin D acts as a hormone and receptors are found in every tissue of our body, it acts on over one thousand different genes! It influences our genes through a process called transcriptional regulation. Simply put, this means it has the ability to turn on or off certain genes in the body.
Vitamin D is a crucial vitamin that’s actually three different vitamins: D1, D2, and D3. The body produces Vitamin D naturally, which can be enhanced by sunlight. Healthline also has a great list of several important benefits of Vitamin D, including:
- Supports the immune system
- May help prevent heart disease
- It may help with mood disorders such as depression
- Supports healthy weight management
- May help prevent and manage IBD
Why is Vitamin D important in IBD?
Recent studies have found a link between IBD and Vitamin D deficiency. In an article in Current Opinion in Gastroenterology, the author describes Vitamin D as “more than just a supplement” and goes on to make several points.
- Vitamin D plays a protective role in gut health
- Up to 30-40% who suffer from IBD also have Vitamin D deficiency
- Low levels are associated with increased disease activity
- Vitamin D may have a positive impact on the gut microbiota
As mentioned previously, vitamin D plays an important role in regulating the immune system. It does so by helping both innate and adaptive immunity and inflammation, increasing anti-inflammatory compounds called cytokines and decreasing those that cause inflammation.
Vitamin D receptors are also found in mucosal immune cells and the intestinal epithelium, as it plays an important role in maintaining mucosal gut barrier integrity (19).
Ultimately, adequate vitamin D is associated with:
- Improved and reduced frequency of IBD symptoms
- Decreased risk for flares
- Reduced risk of IBD onset, particularly in Crohn’s Disease
- Regulation of immune function
- Reduced permeability of intestinal immune cells
- Improved gut barrier function
- Attuned intestinal microbiota
- Improved bone and muscle function
- Decreased risk of colorectal cancer
How do I know if I’m low in Vitamin D?
The best way to figure out if you are low is to do lab work to check for deficiency. However, there are some common signs of deficiency to be aware of.
Signs and symptoms of vitamin D deficiency include:
- Stress fractures
- Chronic pain
- Muscle weakness/poor recovery from exercise
- Frequent upper respiratory tract infections
- Increased risk of flare
The Institute of Medicine suggests 600 IUs per day for those between ages 19 and 50. However, this recommendation doesn’t take into consideration the challenges those with IBD often have with the absorption of vitamin D and the decreases in vitamin D that often occur with having long-term inflammation.
Risk factors associated with vitamin D deficiency include:
- Amount of UV exposure (staying indoors, and use of sunscreen and clothing)
- Ethnicity (skin pigmentation)
- Age
- Certain medications (antacids or prednisone)
- Low vitamin D in the diet
- Chronic inflammation (raises demand)
Here at The Crohn’s and Colitis Dietitians, we like to try and get accurate levels for vitamin D for those we work with one on one. The commonly measured form of vitamin D used to assess and monitor status is 25(OH)D. We like to see serum values between 50 and 80 nmol/L.
Can we get enough Vitamin D through food?
If you are not deficient and do not have an increased risk for low vitamin D, getting enough through the diet is possible.
However, If you are deficient in vitamin D, you’ll need to supplement with the correct dose.
Food sources of vitamin D are fairly limited. There are some known vitamin D food sources including:
- Fatty fish like salmon (570 IUs)
- Fortified drinks (120 IUs)
- UV exposed mushrooms (366 IUs)
The most potent source of vitamin D is through 5-10 minutes of direct sunlight in midday, however for many that is not a viable option. UV exposure is also significantly manipulated by things like latitude, clothing, skin tone, etc. This begs the question, should you supplement?
Should you take Vitamin D?
Ideally, it’s best to work with a doctor or IBD focused dietitian to figure out the best dose for you.
Dosing may vary with many factors including- history of low vitamin D, location, severity of deficiency, and risk factors.
Although vitamin D is considered a fat-soluble nutrient that is stored, it’s important to note that vitamin D is only stored when levels are at 40 ng/mL or higher. This means at severely deficient levels, relying on supplementation is necessary (4).
Vitamin D at a dose of 2,000-4,000 IUs/day is generally safe for those seeking to maintain or prevent deficiency.
Some studies suggest that those with gastrointestinal conditions like IBD or other risk factors may do better with supplementing at a slightly higher dose like 5000 IU. Having said that, it is best to work closely with your healthcare provider to be sure your vitamin D levels are monitored regularly.
Still need help?
Vitamin D deficiency is an important consideration if you’ve got IBD. Low levels can be a roadblock for those of us seeking remission as it is associated with poorer health outcomes, increased risk of flare and severity of flare, and worse response to biologics.
If you need help figuring out how nutrition could help you improve your symptoms and help your medications work better- we are here for you.
As always, a specialized IBD dietitian is an integral part of your healthcare team and we would be honored to be invited into your care. Reach out to us here today to schedule a free initial call!
Resources:
- Ananthakrishnan, Ashwin N., Hamed Khalili, Leslie M. Higuchi, Ying Bao, Joshua R. Korzenik, Edward L. Giovannucci, James M. Richter, Charles S. Fuchs, and Andrew T. Chan. “Higher Predicted Vitamin D Status Is Associated With Reduced Risk of Crohn’s Disease.” Gastroenterology 142, no. 3 (March 2012): 482–89. https://doi.org/10.1053/j.gastro.2011.11.040.
- Ardesia, Marco, Guido Ferlazzo, and Walter Fries. “Vitamin D and Inflammatory Bowel Disease.” BioMed Research International 2015 (April 27, 2015): e470805. https://doi.org/10.1155/2015/470805.
- Barbalho, Sandra Maria, Ricardo de Alvares Goulart, and Rodrigo Gallhardi Gasparini. “Associations between Inflammatory Bowel Diseases and Vitamin D.” Critical Reviews in Food Science and Nutrition 59, no. 8 (2019): 1347–56. https://doi.org/10.1080/10408398.2017.1406333.
- Battistini, Carolina, Rafael Ballan, Marcos Edgar Herkenhoff, Susana Marta Isay Saad, and Jun Sun. “Vitamin D Modulates Intestinal Microbiota in Inflammatory Bowel Diseases.” International Journal of Molecular Sciences 22, no. 1 (December 31, 2020): E362. https://doi.org/10.3390/ijms22010362.
- Cannell JJ, Hollis BW, Sorenson MB, Taft TN, Anderson JJ. Athletic performance and vitamin D. Med Sci Sports Exerc. 2009 May;41(5):1102-10. doi: 10.1249/MSS.0b013e3181930c2b. PMID: 19346976.
- Castro, Francisca Dias De, Joana Magalhães, Pedro Boal Carvalho, Maria João Moreira, Paula Mota, and José Cotter. “LOWER LEVELS OF VITAMIN D CORRELATE WITH CLINICAL DISEASE ACTIVITY AND QUALITY OF LIFE IN INFLAMMATORY BOWEL DISEASE.” Arquivos De Gastroenterologia 52, no. 4 (December 2015): 260–65. https://doi.org/10.1590/S0004-28032015000400003.
- Fakhoury, Hana M. A., Peter R. Kvietys, Wael AlKattan, Fatme Al Anouti, Muhammad Affan Elahi, Spyridon N. Karras, and William B. Grant. “Vitamin D and Intestinal Homeostasis: Barrier, Microbiota, and Immune Modulation.” The Journal of Steroid Biochemistry and Molecular Biology 200 (June 2020): 105663. https://doi.org/10.1016/j.jsbmb.2020.105663.
- Gubatan, John, and Alan C. Moss. “Vitamin D in Inflammatory Bowel Disease: More than Just a Supplement.” Current Opinion in Gastroenterology 34, no. 4 (July 2018): 217–25. https://doi.org/10.1097/MOG.0000000000000449.
- Vitamin D in Inflammatory Bowel Disease: More than Just a Supplement. Current Opinion in Gastroenterology 34, no. 4 (July 2018): 217–25. https://doi.org/10.1097/MOG.0000000000000449.
- Guzman-Prado, Yuli, Ondrej Samson, Jonathan P. Segal, Jimmy K. Limdi, and Bu’Hussain Hayee. “Vitamin D Therapy in Adults With Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis.” Inflammatory Bowel Diseases 26, no. 12 (November 19, 2020): 1819–30. https://doi.org/10.1093/ibd/izaa087.
- Hewison, Martin. “An Update on Vitamin D and Human Immunity.” Clinical Endocrinology 76, no. 3 (2012): 315–25. https://doi.org/10.1111/j.1365-2265.2011.04261.x.
- Jørgensen, S. P., J. Agnholt, H. Glerup, S. Lyhne, G. E. Villadsen, C. L. Hvas, L. E. Bartels, J. Kelsen, L. A. Christensen, and J. F. Dahlerup. “Clinical Trial: Vitamin D3 Treatment in Crohn’s Disease – a Randomized Double-Blind Placebo-Controlled Study.” Alimentary Pharmacology & Therapeutics 32, no. 3 (August 2010): 377–83. https://doi.org/10.1111/j.1365-2036.2010.04355.x.
- López-Muñoz, Pedro, Belén Beltrán, Esteban Sáez-González, Amparo Alba, Pilar Nos, and Marisa Iborra. “Influence of Vitamin D Deficiency on Inflammatory Markers and Clinical Disease Activity in IBD Patients.” Nutrients 11, no. 5 (May 11, 2019): E1059. https://doi.org/10.3390/nu11051059.
- Mouli, Venigalla Pratap, and Ashwin N. Ananthakrishnan. “Review Article: Vitamin d and Inflammatory Bowel Diseases.” Alimentary Pharmacology & Therapeutics 39, no. 2 (January 2014). https://doi.org/10.1111/apt.12553.
- Nic Suibhne, Treasa, Gerry Cox, Martin Healy, Colm O’Morain, and Maria O’Sullivan. “Vitamin D Deficiency in Crohn’s Disease: Prevalence, Risk Factors and Supplement Use in an Outpatient Setting.” Journal of Crohn’s and Colitis 6, no. 2 (March 1, 2012): 182–88. https://doi.org/10.1016/j.crohns.2011.08.002.
- Nielsen, Ole Haagen, Lars Rejnmark, and Alan C. Moss. “Role of Vitamin D in the Natural History of Inflammatory Bowel Disease.” Journal of Crohn’s & Colitis 12, no. 6 (May 25, 2018): 742–52. https://doi.org/10.1093/ecco-jcc/jjy025.
- Parizadeh, Seyed Mostafa, Reza Jafarzadeh-Esfehani, Seyed Mahdi Hassanian, Ali Mottaghi-Moghaddam, Anahita Ghazaghi, Maryam Ghandehari, Mohadese Alizade-Noghani, et al. “Vitamin D in Inflammatory Bowel Disease: From Biology to Clinical Implications.” Complementary Therapies in Medicine 47 (December 2019): 102189. https://doi.org/10.1016/j.ctim.2019.08.023.
- Tabatabaeizadeh, Seyed-Amir, Niayesh Tafazoli, Gordon A. Ferns, Amir Avan, and Majid Ghayour-Mobarhan. “Vitamin D, the Gut Microbiome and Inflammatory Bowel Disease.” Journal of Research in Medical Sciences : The Official Journal of Isfahan University of Medical Sciences 23 (2018). https://doi.org/10.4103/jrms.JRMS_606_17.
- Valvano, Marco, Marco Magistroni, Antonio Mancusi, Debora D’Ascenzo, Salvatore Longo, Gianpiero Stefanelli, Filippo Vernia, Angelo Viscido, Stefano Necozione, and Giovanni Latella. “The Usefulness of Serum Vitamin D Levels in the Assessment of IBD Activity and Response to Biologics.” Nutrients 13, no. 2 (January 22, 2021): 323. https://doi.org/10.3390/nu13020323.
- Yuli Guzman-Prado, MD, MSc, Ondrej Samson, Jonathan P Segal, PhD, Jimmy K Limdi, FACG, Bu’Hussain Hayee, PhD, Vitamin D Therapy in Adults With Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis, Inflammatory Bowel Diseases, Volume 26, Issue 12, December 2020, Pages 1819–1830, https://doi.org/10.1093/ibd/izaa087



0 Comments
Trackbacks/Pingbacks