If you’ve got Crohn’s or Colitis, you may have had anemia at some point or you may find your doctor checking for anemia regularly in blood work.
Anemia is one of the most common reasons for IBD related fatigue and affects around 24% of IBD patients (1). In our practice, we see anemia in almost 50% of our patients.
There are actually several types of anemia related to nutrients like vitamin B12 and folate but half of all anemia cases are related to iron deficiency (1).
Iron plays a major role in:
- The transport of oxygen throughout our body
- Our energy production- mitochondria produce ATP for us (aka energy)
- Iron plays a critical role in repair of tissues through making DNA repair enzymes (2)
- Cognitive function, memory and problem solving
- Supporting our immune system’s initial protective defense (3, 4)
As you can see from the list above, having adequate iron in the body is crucial for energy, our immune system and being able to perform day to day activities.
When it comes to IBD specifically, we also need iron for repair of tissue which is important since during a flare our immune system causes damage to digestive tissue.
When you are anemia you might notice symptoms like:
- Fatigue or general tiredness
- Sensitivity to cold
- Restless leg
- Trouble focusing
- Trouble with decision making
- Slower recovery
- Paleness
- Irregular heartbeat
- Dizziness
- Cold hands and feet
- Trouble breathing
- Chest pain
So what can you do if you’ve got anemia?
I’ve laid out what I think are the 5 most important considerations.
5 steps to solving IBD Anemia:
1. Work with your doctor to uncover the root causes
It’s important to have an understanding of the biggest driver of your anemia.
This can vary from person to person.
Gastrointestinal bleeding and inflammation are the common drivers of IBD anemia when someone is in a flare.
If you are in clinical remission and still have anemia- sometimes we need to look further at your intake and check for genetic conditions that could drive anemia.
For those who mensturate, heavy periods can also contribute to anemia.
To uncover what the root concerns are for your anemia, your doctor or dietitian might run lab tests to check for inflammation by running markers like CRP, fecal calprotectin or sedimentation rate.
2. Treat the root issue as best as possible
Just taking iron alone and not considering what’s causing the anemia won’t always yield positive results.
If inflammation or bleeding is the cause of the anemia, you may need to bring in strategies to address the root cause as well. This might include medication, herbal anti-inflammatories or dietary strategies.
In some cases, when anemia is severe enough- iron infusions or transfusions may even be required. In these cases, medication, supplemental and dietary strategies alone will not be enough to support you.
To detect which route might be most effective for treatment of anemia, your health care provider might run lab tests to look at hemoglobin, hematocrit and ferritin (iron storage).
If you are at risk for low iron levels, occasional supplementation might be the best option. We regularly help those with anemia or at risk for anemia in our practice. Those with higher risk include:
- Those on vegan diets
- Athletes or heavily active individuals
- Those diagnosed with Crohn’s or Colitis
- Those that menstruate
3. Supplement with the right dose, frequency & type of iron
If anemia isn’t severe enough to require infusions or transfusions- supplementation could be the best fit.
However, how can you tell what type of iron supplement is best to take?
In my professional opinion, the best type of iron supplement for Crohn’s and Colitis is one that meets this criteria:
- Is well absorbed
- Reduces the chance of gut irritation & constipation
- Is cost effective
There are many types of iron available on the market- iron sulfate, iron oxide and several others.
My personal favorite is iron bisglycinate.
I prefer iron bisglycinate since it has higher absorption rates and is gentle on the digestive tract.
To get the right dosing- work with your doctor or IBD focused dietitian (like me) to find the correct dosing for you.
It’s important to test and not guess- since it’s possible to take too much iron too.
4. Enhance absorption
Other than taking a higher absorption iron, what other ways can we enhance iron absorption?
Taking Vitamin C rich foods with meals containing plant based (non-heme) iron sources can improve iron absorption by up to 67% (5).
Food sources of vitamin C include citrus fruits, dark green leafy vegetables, bell peppers, melons and strawberries.
However, when it comes to supplementation of iron some studies indicate that the addition of vitamin C doesn’t seem to improve absorption in the same way (6).
Pairing food sources of iron with vitamin A and beta carotene has also been shown to improve absorption by up to 200% in some studies (7).
Beta-carotene and vitamin A rich foods include carrots, sweet potatoes, kale, spinach, squashes, cantaloupe, apricots, red peppers, oranges and peaches.
It’s important to recognize that iron isn’t the only nutrient that’s important with anemia- many nutrients like copper and B vitamins are supportive and synergistic with the treatment of anemia.
5. Retest & Troubleshoot anemia
If you are still struggling to treat anemia and aren’t seeing good results with the approaches above- there are still other strategies you can consider to help treat it.
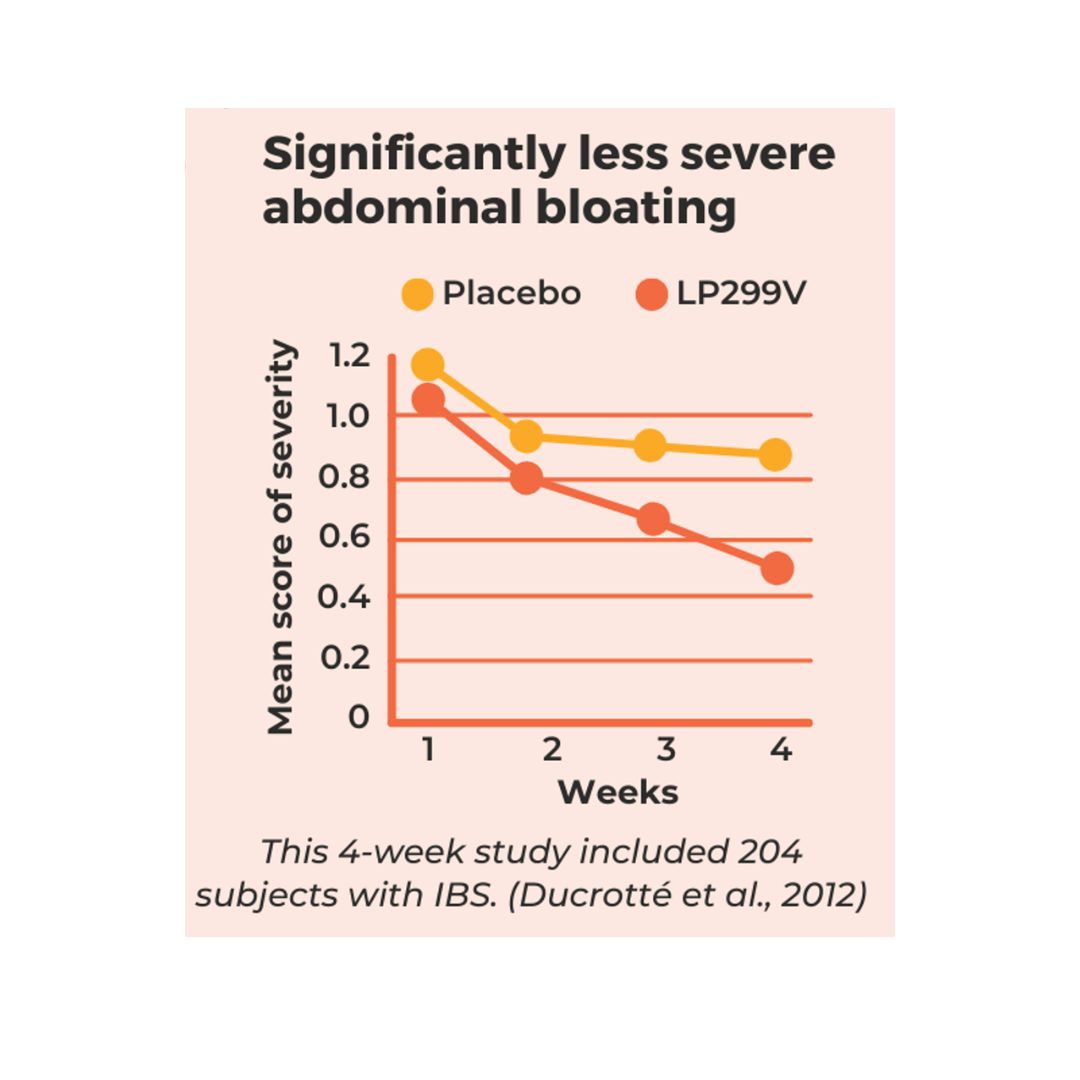
There is some research that suggests gut bacteria changes might contribute to bacteria consumption of iron which impedes iron absorption. Combining iron with Lactoferrin is a great way to bypass this concern and help support absorption of iron (8, 9, 10).
Another study also suggests that skipping days rather than taking iron daily can actually make cells more responsive to absorbing iron (11). You can talk to your doctor or IBD dietitian about incorporating a strategy that spaces out iron intake to enhance absorption.
Also, if you are an athlete or fairly active, you should consider your workouts as well, taking iron in the morning or within 30 minutes after a workout can potentially increase absorption (12, 13).
After workouts, something called hepcidin increases steadily which blocks iron from absorption.
However, timing iron intake right after a workout can bypass this system and potentially help as well.
Final Note:
If you are not certain how to best address your fatigue or ongoing anemia- apply for a call with us.
Curious about other types of supplementation for IBD? Check out our previous blog on 4 supplements with evidence for IBD.
Do you know the different types of remission? Is it IBS or IBD- find out more on our blog: How to know if you are in remission
References





0 Comments
Trackbacks/Pingbacks