Have you ever wondered what to eat in a microscopic colitis flare up? Microscopic colitis, a chronic inflammatory bowel condition, can be quite challenging for those who experience its primary symptom – recurrent episodes of diarrhea. This unpredictable condition can lead to flare-ups at unexpected times, causing significant disruptions to one’s daily life.
During such episodes, adopting a suitable diet alongside prescribed medications can help manage symptoms more effectively. In this article, we will provide you with a round-up of foods to prioritize during a microscopic colitis flare-up, promoting better gut health and easing your discomfort.
What to Eat in Microscopic Colitis Flare-up
In this blog post, we delve into the essential aspects of microscopic colitis, a chronic inflammatory bowel condition that can lead to persistent watery diarrhea and abdominal discomfort.
By providing an in-depth understanding of the condition and its symptoms, we aim to empower our readers to manage microscopic colitis effectively. Throughout this post, we will discuss the types of microscopic colitis, potential triggers, and various treatment strategies, including dietary modifications and medication usage.
Additionally, we will share valuable insights on lifestyle adjustments that can alleviate symptoms during a flare-up. Keep reading to gain a comprehensive understanding of microscopic colitis and learn practical tips for managing this condition.
What is Microscopic Colitis
Microscopic colitis is a type of chronic inflammatory bowel disease that affects the large intestine characterized by an over reactive immune system.
Symptoms of microscopic colitis include persistent watery diarrhea, abdominal pain, and bloating. The two types of microscopic colitis are collagenous colitis and lymphocytic colitis.
Lymphocytic colitis causes white blood cells called lymphocytes to increase in colon tissue where as collagenous colitis is where a thick band of collagen grows in colon tissue.
Unlike other forms of inflammatory bowel disease, such as Crohn’s disease or ulcerative colitis, microscopic colitis doesn’t have visible inflammation or ulcers in the colon. Instead, the inflammation is only visible under a microscope.
The condition is relatively common, affecting approximately 100 out of 100,000 people each year, with a higher prevalence in women and individuals over the age of 60.
Microscopic colitis can significantly impact one’s quality of life, as the recurrent episodes of diarrhea and accompanying symptoms can be debilitating and unpredictable.
It’s important to note also that with microscopic colitis there are higher rates of celiac disease as well which if diagnosed will require a gluten free diet.
What Triggers Microscopic Colitis Flare-Up
Identifying the triggers of microscopic colitis flare-ups can be challenging due to the variation in individual experiences. Before we dive into what triggers Microscopic colitis, it’s important to distinguish that there are 3 types of triggers.
The 3 types of triggers:
- Inflammatory Diet Pattern Triggers
- Symptom Triggers
- Stress, Trauma & Fear Triggers
Inflammatory diet pattern triggers are things within the diet over time that can increase risk of inflammation in IBD. It’s important to note that things listed in this category might not trigger symptoms, but we do know they can increase overall risk of flares and inflammation over time.
We’ve listed a list further into this blog, but check out our e-books for a more thorough understanding than a blog can provide.
Symptom triggers on the other hand are not linked with increasing risk of inflammation flares. These are often things that can increase symptoms but aren’t causing harm. Often, symptom triggers can also change with time especially with small incremental steps that encourage positive changes to the microbiome.
In fact, when we work one-on-one with our patients, we help IBD patients add a variety of foods back without triggering symptoms. Symptom triggers vary a lot person to person. We cover them more in depth in our flare friendly e-book & meal plan and microscopic colitis e-book.
Stress and anxiety are other potential triggers, as they can disrupt the gut-brain connection and negatively impact gastrointestinal function regardless of wether or not there is inflammation present.
In addition, many people with IBD may have fear or trauma triggers with food. Many with IBD experience legitimate fear with food which can lead to restrictions in the diet and can complicate their relationship with food.
What Should You Eat If You Have Microscopic Colitis Flare-Up
Have you ever notice that most blogs only focus on things to avoid? Often you are left wondering what the best foods to eat are. Below is a list of the top things to prioritize.
Most people do well with smaller particle size foods in flare ups such as cooked vegetables, soups, smoothies and soft consistencies.
Here are four food categories to prioritize during a flare-up:
Electrolytes and Appropriate Fluids
Diarrhea of more than six times per day can lead to dehydration, so it’s crucial to replenish fluids and electrolytes. While often people go for sports drinks, these are often higher in sugar but lower in other minerals. If you are very low in electrolytes, you may need to opt something like Cure or Bumbleroot for staying properly hydrated.
While often people go for sports drinks, these are often higher in sugar but lower in other minerals. If you are very low in electrolytes, you may need to opt for
As an alternative, you can also try making your own version using coconut water which is rich in potassium and adding some salt.
Souble Fibers & Resistant starches
Soluble fibers can be helpful at soaking up excess moisture and helping to slow the transit time to lessen the frequency and urgency of bowel movements. In addition, encouraging some fibers can help encourage butyrate production which we know is key to inflammation reduction and repair of the intestinal wall (among helping with many other things).
Oat bran, cooked and cooled potatoes and rice, slightly green bananas are great starting places for incorporating soluble fibers and resistant starches.
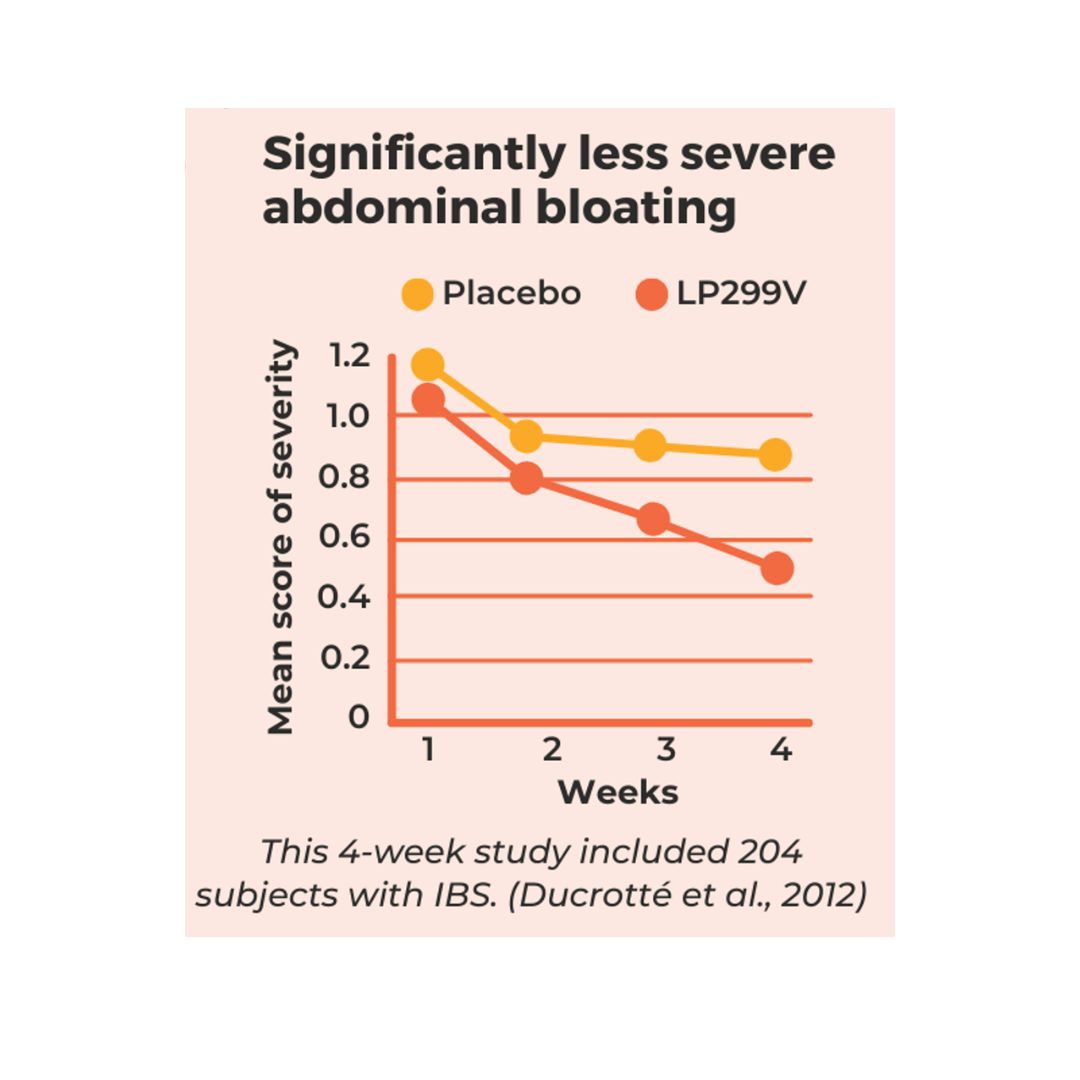
Back to Balance plus is our favorite go-to recommendation for reducing frequency and urgency of bowel movements in a more systematic way. It includes a very well tolerated and easy to incorporate soluble fiber that completely dissolves in water.
Back to Balance plus has great evidence to support it’s use after 4-6 weeks of use and also helps encourage the growth of lactobacillus and bifidobacteria. You can read more on the research here.
Omega-3 Fatty Acids
Omega-3 fatty acids can be helpful with reducing inflammatory cytokines and can help encourage the right gut environment (1).
Although many studies have shown that Omega-3 fatty acids may regulate and attenuate the inflammatory processes and lead to remission of IBD, you may have seen mixed reviews on how strong this research is. In my opinion, this likely due to the variability in the doses and way of delivery (1).
From what we know about them as a whole, they offer many positive benefits and are easy to get in. Your best sources are halibut, mackerel, herring, salmon, sardines and anchovies. The best plant based sources are walnuts, flax and chia seed.
Smoothies to add color
Smoothies offer a few things that are a great fit. The first is that it’s a great way to easily bring in fruits and vegetables into the diet with less symptoms.
If you are able to pair your smoothie with a protein source like soy milk and maybe a fat like almond butter – this pairing can make a great meal too when you don’t feel up for eating.
Remember to start with small serving sizes and go “low and slow” with introducing new foods.
What Are The Worst Foods For Microscopic Colitis
It’s important to remember that it’s not a single food that causes harm- even with things on the inflammatory list. It’s truly the pattern of eating we need to consider when it comes to increasing the risk of flare ups.
Another thing that’s just not talked about enough is that it’s not just inflammatory food patterns that put IBD patients at risk – it’s also heavy restirction. Malnourishment is a risk factor for those with IBD that can negatively influence recovery and response to medication.
In addition, long term restriction can even impact the speed at which foods pass through the digestive system which can actually increase symptoms.
We define malnourishment as anyone who meets any of the criteria below:
- Skipping meals to avoid symptoms more than twice weekly
- Unintentional weight loss of more than 10 lbs
- Feeling as if you have less than 10 safe foods
- Feeling significant fear and anxiety at meal time which impacts your food choices
- On a restrictive diet longer than intended without oversight by a dietitian (such as low fodmap diet, low residue)
If you feel like you meet any of the criteria above, you aren’t alone. Close to 80% of those with IBD experience disordered eating patterns that lead to malnourishment. This is complicated by the fact that information online is often conflicting and most patients aren’t referred to a IBD dietitian.
If you meet the criteria above you may need guidance from a IBD focused registered dietitian. You can find ways to work with us here.
Here’s a list of some of the worst food patterns for microscopic colitis:
- Malnourishment & skipping meals can delay recovery and lower response to meds
- Diets that are low or restricted in fiber and plants
- A diet high in red and processed meats
- Diet high in myristic acids and saturated fats (dairy products, coconut oils)
- High in fillers like nitrates, carageean, polysorbate 80, carboxymethylcellulose
I pulled this from multiple studies overtime and also the IOIBD guidelines. This isn’t a full list of everything that’s helpful to know. You can find more in our flare friendly e-book & meal plan and microscopic colitis e-book.
It’s essential to note that individual food tolerances may vary, and some people may tolerate small amounts of these foods without long term effects. Also, remember that many of these food patterns may not cause symptoms directly but can increase risk of flare up long term.
If you aren’t sure where to start when it comes to nutrition and managing your microscopic colitis long term, please reach out and work with us!
Other articles:
Ulcerative colitis food list – https://crohnsandcolitisdietitians.com/ulcerative-colitis-food-list/
What to eat – https://crohnsandcolitisdietitians.com/microscopic-colitis-food/
References:
Marton LT, Goulart RA, Carvalho ACA, Barbalho SM. Omega Fatty Acids and Inflammatory Bowel Diseases: An Overview. Int J Mol Sci. 2019 Sep 30;20(19):4851. doi: 10.3390/ijms20194851. PMID: 31574900; PMCID: PMC6801729.





0 Comments
Trackbacks/Pingbacks