Having a lifelong condition like IBD can be extremely challenging. As well as managing physical symptoms, there are many emotional consequences that can even impact how well you are able to cope with the disease.
Not suprisingly, there is a high prevenance of depression and anxiety for those with IBD as compared to the general population.
In my own personal experience, the impact of IBD on my quality of life in the first year of my diagnosis was just as difficult to navigate as the symptoms I experienced.
This is one of the reasons IBD and mental health is a priority for us to discuss when we work with patients.
This is also why we have our podcast Gut Feelings – where we do also sprinkle in our personal stories and experiences with IBD. We cover many topics including the intersection of IBD and mental health.
Our most popular episode is on the topic of gut brain interaction and the gut brain axis. It features Dr Navidi from GI psychology. It’s our most popular episode so far.
My biggest take-away from our conversation was how much we can’t ignore the gut brain interaction and the role that plays in symptoms and even disease trajectory. We already know that long term-perceived stress can increase risk of flare up.
And because they are so connected, this also presents an opportunity for us to also:
- Support our gut to impact mental health
- Support our mental health to impact our gut
- Bring in strategies to help encourage better stress resilence
We can’t take stress away, but we can change our response to it which can in turn change how it impacts us.
My favorite TED talk ever is called making stress your friend. You can apply the lessons from the research presented in it by incorporating your own mental health tools to become more resilient to the stresses brought on by IBD and in turn lower your risk of flare-ups.
Here we share how to support your recovery by understanding the impacts of stress and becoming more resilient.
IBD and Mental Health
IBD, or Inflammatory Bowel Disease, is a chronic condition that causes inflammation of the digestive tract. This can be extremely painful and cause many physical symptoms:
- Severe pain and cramping
- Bloody stools
- Fatigue
- Joint pain
- Diarrhea
- Loss of appetite
IBD flare-ups can often be sudden. They can happen at inconvenient times or when you least expect it, leading to feelings of overwhelm, stress, and shame. You may also experience the various stages of grief after diagnosis including denial, bargaining, and depression.
Those with IBD have a higher risk of developing anxiety and depression, while prolonged stress can triple the risk of flare-ups. It’s therefore incredibly important to stay in tune with your emotional health and learn to manage both physical and psychological symptoms.
Diet for IBD Flare Ups
If you’ve ever done any research on Diets for IBD, you’ve probably come across the mediterranean diet as being in the lead for the best approach overall for reduction of inflammation markers and symptom reduction.
The reason I think that the mediterranean diet has gotten the attention it has in the research is that it includes omega 3’s, is rich in herbs, beans, color and fiber. If you are already about to close this blog because those feel out of reach – consider working with us.
Our specialty is helping people expand their diets without triggering symptoms – even in flares, even with strictures and without making it overly complicated. We will help you come up with a personalized plan for reducing symptoms that fits you and your IBD.
We are good at what we do because we believe patients with IBD deserve answers, tools to help relieve symptoms and compassionate care. And now we even have 3 ways you can work with us. If this interests you, act now because we regularly fill up our schedules fast.
Tell me more than just do the Mediterranean diet
As an IBD nutrition researcher myself, I’m always asking why things work the way they do. If you are like me and like to get into the details of what exactly works and why.
And if you are someone that hears “just follow the mediterranean diet” and you immediately wonder how many different versions of that there are and also question why only this culture was studied over other cultures – well then you are in the right place.
You might be left with questions like:
- What if you are struggling to get in fruits and vegetables?
- What if only 5 foods feel ‘safe’ for you?
- What about preservatives, emulsifiers, and additives?
- What about red/processed meats and dairy? If problematic, how much is ok?
- What about gluten and alcohol? What does the research say?
- What about supplements? Are there any that are evidence based?
- How about other cultural diets outside of mediterranean? Why aren’t those studied?
If any of these questions are coming up for you, you can search our website and probably find a lot of the answers. Or if you’d like a short cut, we have one just for you.
Our Flare e-book is packed with answers to your questions as well as practical insights into how to implement our suggestions. We also include evidence based strategies to target symptoms like bloating, abdominal pain, diarrhea, urgency, constipation, fatigue and more.
A major bonus with the flare e-book is that it comes with a meal plan and IBD friendly recipes! We have gotten so much positive feedback from it so far from both newly diagnosed people and those who’ve had IBD for 30 years or more.
While the research spotlight seems to only be on the mediterranean diet at the moment, I’ve been inspired by the work of Dr Oriana Damas who has looked further into the importance of personalized nutrition and including culture.
Dr Damas has also presented on IBD and Hispanic/LatinX dietary patterns which has brought light to the fact that there isn’t only one pattern that works.
Take-away Tips for Diet during an IBD Flare Up
It can be overwhelming to know where to start when you are in a flare-up. Just like you go to your gastroenterologist for medication and next steps and go to your therapist when life gets overwhelming, an IBD dietitian can help you feel less overwhelmed with your nutrition.
So if you need help, don’t be afraid to get it! We are here for you. If you are malnourished (ie. only have 5 safe foods, or skipping meals to avoid symptoms) – then an e-book and blog probably won’t cut it. Use our help if you need it.
Some Take-away Tips:
- If expanding your diet feels like too much – work with an IBD dietitian
- If you can’t work with us, start with our Flare E-book
- Blending and cooking changes the particle size of food and can help with tolerance
- We know color, omega 3’s and diversity is important for reducing flare risk
- Not including fiber is associated with a higher likelihood flares long term
- Emulsifiers like polysorbate 80, carboxymethylcellulose and carrageean continue to show up in research as not good for gut health in IBD
- When it comes to inflammatory things – it’s dietary patterns over time that matter rather than one time food exposure
- It’s important to prioritize getting enough (meeting your baseline needs) over restricting
How to care for your mental health to support IBD recovery
It can be hard to stick to your treatment plan if you feel down and unmotivated. So make sure to understand how to spot signs of stress and what to do next.
If you’ve got friends and family members that can be there for you when you are in a flare or struggling, don’t be afraid to ask for what you need. Often those that love you, want to help and would love for you to tell them how to.
It may also be helpful to get help from a therapist when things are tough. A therapist can help you process what’s happening. And give you tools for how to better cope which can build stress resilience.
What do we mean by stress resilience?
Everyone has a different perception of what stress is and what triggers their stress response. For some, it could be an important work call. While for others, it can be the thought of a flare-up happening in the future.
While it can be difficult to identify what stress and anxiety look like to you, there are common symptoms:
- Nervousness
- Restlessness
- Dissociation and shutting down
- Panic and fear
- Feeling a lack of control
These emotions can also overlap with depression often characterized by low mood, feelings of hopelessness, or in severe cases, thoughts of suicide. If you have any of these symptoms please contact 1-800-273-8255.
How stress affects your body and the risk of a flare-up
There are a number of psychological and physiological changes that happen in our bodies when we are stressed, each of which contributes to IBD flare-ups.
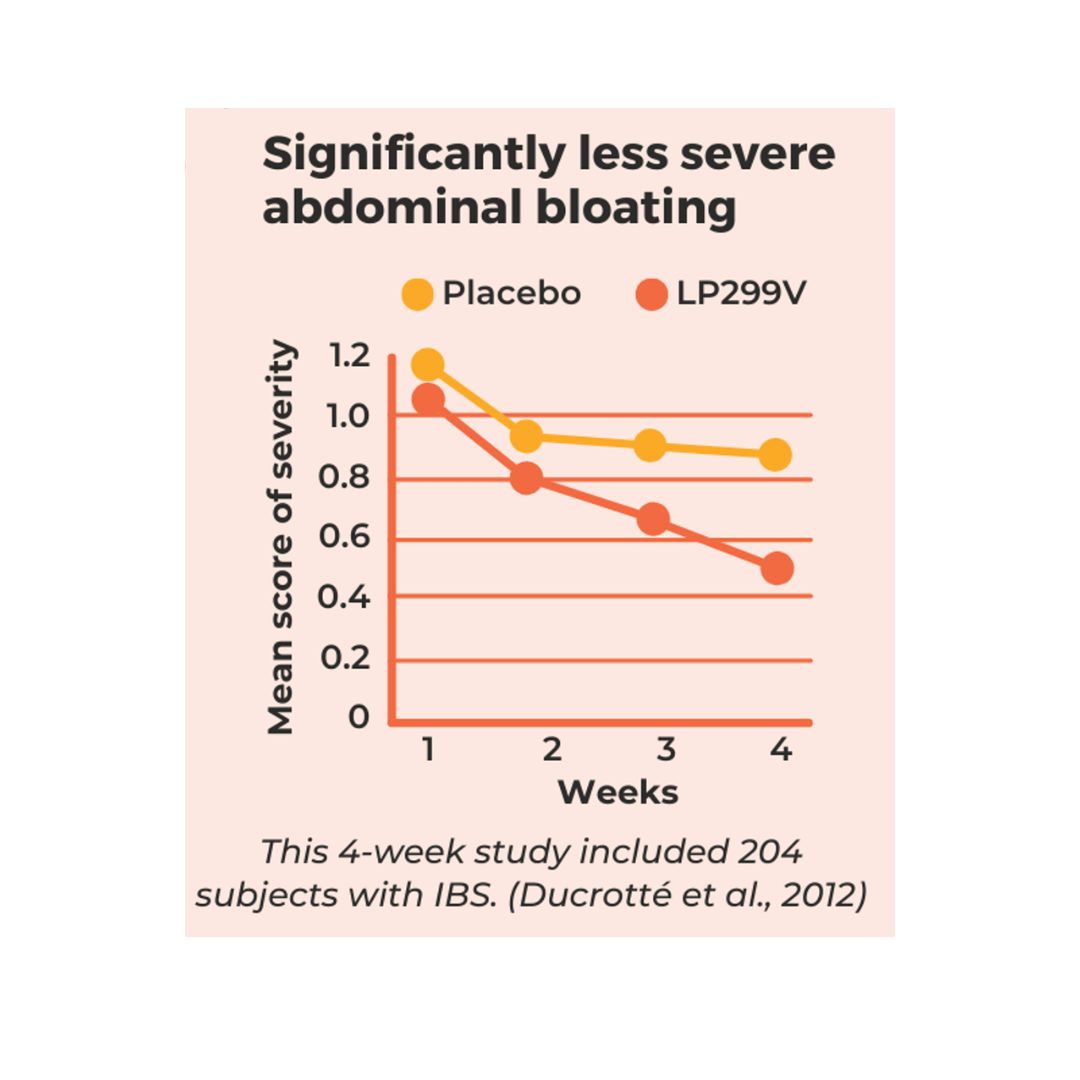
We also know that long-term perceived stress can actually triple our risk of IBD flare! Here is how it works below.
Your brain becomes hyperactive
The amygdala part of the brain is responsible for emotions such as fear and aggression. During stress, this area becomes hyperactive and can lead to exaggerated responses and reactions.
Continuous stress can also impact the prefrontal cortex, the part of your brain that is responsible for decision-making and judgment. When in a state of fight or flight, this makes it harder for us to think clearly, make appropriate decisions, and cope with flare-ups.
Disruption to the gastrointestinal tract
If you’ve ever felt butterflies in your stomach or felt nauseous before an interview, you’ll have experienced the gut’s sensitivity to emotion. This is because the gut and brain are physically connected and communicate with each other through the vagus nerve.
When you feel disconnected, anxious or stressed, the brain sends signals to the gut resulting in disruption to your gastrointestinal tract known as dysbiosis. When this happens, your gut’s bacteria becomes unbalanced, often resulting in a sense of urgency (needing the toilet quickly) or slowing down (such as constipation).
High c-reactive protein (CRP)
When we experience stress longer term, we tend to see higher inflammatory markers, one of which is c-reactive protein (CRP). Produced by the liver, high levels of CRP indicate inflammation in the body.
Each of these factors can disrupt your digestive tract and gut bacteria, which if not controlled can affect how well you respond to treatments and your risk of flares.
How to be more stress-resilient
While stress can’t be avoided, there are various ways you can train your mind to become more resilient and comfortable with triggering situations.
- Accept your stresses – it’s normal to want to ignore any signs of stress or pretend it’s not happening. However the more you resist, the more it will persist! If you ignore symptoms and internalize your stress, it will only get stronger and cause more intense flare-ups in the long run. It’s much healthier to embrace what you are feeling and accept what is happening to your body. Take deep breaths and calmly check in with yourself.
- Adapt how you perceive stress – many of us have experienced the feeling of being stressed… because we are stressed! Break this vicious cycle by reframing your thoughts in a positive light. Instead of worrying that your heart rate has increased, consider how it shows your body’s strength.
- Find your stress reliever – from walking and meditation to journaling or dancing to your favorite music… there are plenty of therapeutic ways to destress. Find yours and make time for enjoyment each day to help release those psychological and physiological symptoms.
How to cope with IBD flares through support
The number one way to cope with flare-ups and discomfort is to get support. When we feel accepted, understood, and loved our brain releases oxytocin. Sometimes known as ‘the love hormone’, it plays a significant role in regulating stress responses and reducing our blood pressure.
A hug automatically releases a boost of oxytocin. But you don’t need physical support to benefit from this stress-relieving hormone.
Start by talking to people who understand what you are going through. There are plenty of support groups where those with IBD can share experiences and relate to one another. Being heard is the first step to feeling supported.
Therapy is also extremely beneficial to support those with IBD. It can help you to deal with stress and emotions but also to find the words to explain what you are going through to others. You could also share our guide to supporting a loved one with IBD with friends and family to help them understand your disease.
Lastly, remember to accept help from your loved ones. You can’t think about decision-making in the same way when your body is in pain or stressed. Don’t feel embarrassed to ask for practical support.
Get support with your IBD and mental health
Living with IBD can be difficult, but there is a wealth of support that can help you from groups and resources to expert professionals.
As specialists in IBD, the Crohn’s and Colitis Dietitians team are here for you. Our personal experiences with the disease mean we know first-hand the impact it can have on the body and mind – and our nutritional therapy can help you with both.
Contact our team today and get the support you deserve.





0 Comments
Trackbacks/Pingbacks