An Inflammatory Bowel Disease (IBD) flare is a scary spot to be in. We often want to immediately fix an IBD flare with the quickest solutions possible so we can get back to our normal lives. As much as a quick solution would be nice to have, our best resource is to support our bodies as much as possible to prevent a colitis or crohn’s flare.
Let’s take a look at some ways you can help minimize your risk of a flare as well as explore how food, stress, and medications can be beneficial to monitor to reduce your risk of flare in IBD.
How Do You Fix an IBD Flare?
What triggers an IBD flare?
If you have IBD there’s no doubt you’ve experienced a flare before. A flare is classified as the return or worsening of symptoms.
Symptoms can include:
- Diarrhea
- Multiple trips to the bathroom
- Urgency
- Fatigue
- Abdominal pain
- Weight loss
- Bloody stools & rectal bleeding
- Nausea & vomiting
All of the above is something no one ever wants to experience, but are there certain things that specifically contribute to the onset of a flare? Well…yes and no.
Can the food we eat cause a flare?
People living with IBD may experience symptoms around certain foods throughout different stages of the state of their disease. However, symptoms do not automatically mean there is a flare brewing.
Dietary choices can go a long way for someone with inflammatory bowel disease. When looking at diet, it’s best to choose something sustainable and let go of the “all or nothing” approach. Dietary patterns can help in reducing inflammation and improving symptoms.
In the most recent IOIBD guidelines it was found that the following foods/food practices were more likely to cause flares:
- High saturated fat foods, specifically those containing myristic acid (ex: butter, palm kernel oil, and coconut oil)
- Ultra processed foods with additives and emulsifiers like polysorbate-80 and carrageenan
- Alcoholic beverages
- A low fiber diet
By reducing your intake of highly processed foods and saturated fats as well as alcohol while increasing fiber, you can help reduce your risk of flare! Importantly though, it’s not about a single day of eating. The whole dietary pattern helps protect us from a flare and can help lengthen the time from a future flare occurring.
It’s also important to note that there is not one diet out there for everyone and it is best to take an individualized approach to your best health. The Crohn’s and Colitis Dietitians can help determine what dietary strategies and patterns are best for you and your IBD.
What does a low inflammatory diet pattern look like?
Our approach at Crohn’s & Colitis Dietitians is to help decrease inflammation by improving the health of the gut lining. This is especially helpful when trying to fix an IBD flare situation.
We work with our clients to achieve this by:
- Increasing fiber intake
- Choosing antioxidant rich foods
- Including omega-3 rich foods more often
- Reducing stress
Increasing fiber intake
Fiber can be found in fruits and vegetables, and whole grains. When fiber is increased in the diet, a short chain fatty acid called butyrate is produced. Butyrate is shown to help decrease inflammation and reduce oxidative stress in the colon. In those with Crohn’s who chose to eat a high fiber diet it was found that 40% were less likely to flare (1)!
Having smaller meals more frequently in your day can be a helpful way to add in extra fiber while decreasing the work your gastrointestinal tract has to do at one time. Don’t forget to go low and slow, and drink plenty of water when increasing fiber.
Keeping a food journal is another helpful tool to determine if there are any foods contributing to unwanted symptoms.
Choosing antioxidant rich foods
Antioxidants can prevent damage to our cells. Antioxidants work their magic by neutralizing harmful free radicals in our bodies. Free radicals can be caused by smoking, environmental pollutants, and chemicals. Introducing antioxidant rich food like berries, leafy greens, green tea, and citrus fruits help provide another protective layer to prevent damage to our cells.
Including Omega-3’s more often
Omega-3 fatty acids are a type of fat known for its health benefits. In IBD specifically, omegas can prevent joint pain, decrease inflammation, and help protect you against flares. Increase your intake of omega-3 foods by including fatty fish like salmon, trout, and sardines, as well as nuts (especially walnuts), flaxseed, and leafy greens throughout your week.
If you are looking for more specifics on what to eat with Crohn’s Disease or Ulcerative Colitis, we have plenty of blogs to view or you can schedule a call for more individualized support!
Does stress contribute to flares?
Stress does not cause IBD, but long-term stress can aggravate symptoms and triples your risk of a flare up (2). There are both short-term (acute) and long-term (chronic) types of stress. An example of short-term stress is when you get frustrated by getting stuck in traffic. An example of long-term stress is when the challenges and pressures of work or a relationship consumes you.
Productive ways to manage your stress level and mental health may include:
- Setting aside an hour a week to practice self care (examples: yoga, a hot beverage with a friend, hiking, etc.)
- Practice breathing exercises like box breathing
- Enjoying your favourite tea and a good book
- Spending quality time with family and friends
How do medications stack up?
There tends to be a lot of confusion and misunderstanding about medications for IBD. Many people fear them and wonder if they should be used at all. But, it’s much safer to take medications to control inflammation rather than let it continue to mount.
If you are prescribed medication for your IBD it is best to follow exactly how your doctor and pharmacist suggests to take it for it to work best in your body and to avoid any adverse effects. Doing so will help fix an IBD flare quickest.
One way for your gastroenterologist to determine if the prescribed medication is effective is through lab work. This may include a variety of bloodwork and stool samples. Common tests include fecal calprotectin, CRP, drug level status, and nutrient status. For more information on labs to ask for, see our past blog post here.
But, what about other routine medications for pain or bacterial infections?
Non-steroidal anti-inflammatory (NSAID) drugs such as aspirin, naproxen, and ibuprofen have the ability to cause flares and should be avoided. Instead, acetaminophen can be used for pain management, but be sure to discuss this with your doctor.
Antibiotics are often used for treatment in Crohn’s patients with fistulas, pouchitis, and abscesses, but are not used for treatment in those with Colitis. Antibiotics have the potential to trigger symptoms in IBD which is why it is important to only use them when there is an infection present and under supervision of your doctor.
Key Takeaways: Minimizing your risk of flare
There are always going to be strategies out there to support your health and we hope you can take a strategy away from this blog to improve your gut health. If you are still looking for a place to start, check out these quick tips below!
The best ways to minimize your risk of flare are to:
- Take medication as prescribed by your healthcare team.
- Find ways to add fiber to your day. Start small! Include 1 extra serving of vegetables to your lunch or supper plate.
- Learn to manage stress in a way that best suits you!
- Stay up to date with lab work.
Do you need further support for your gut health in 2023? Schedule a free, no-pressure call to discuss ways we can support your IBD journey this year!
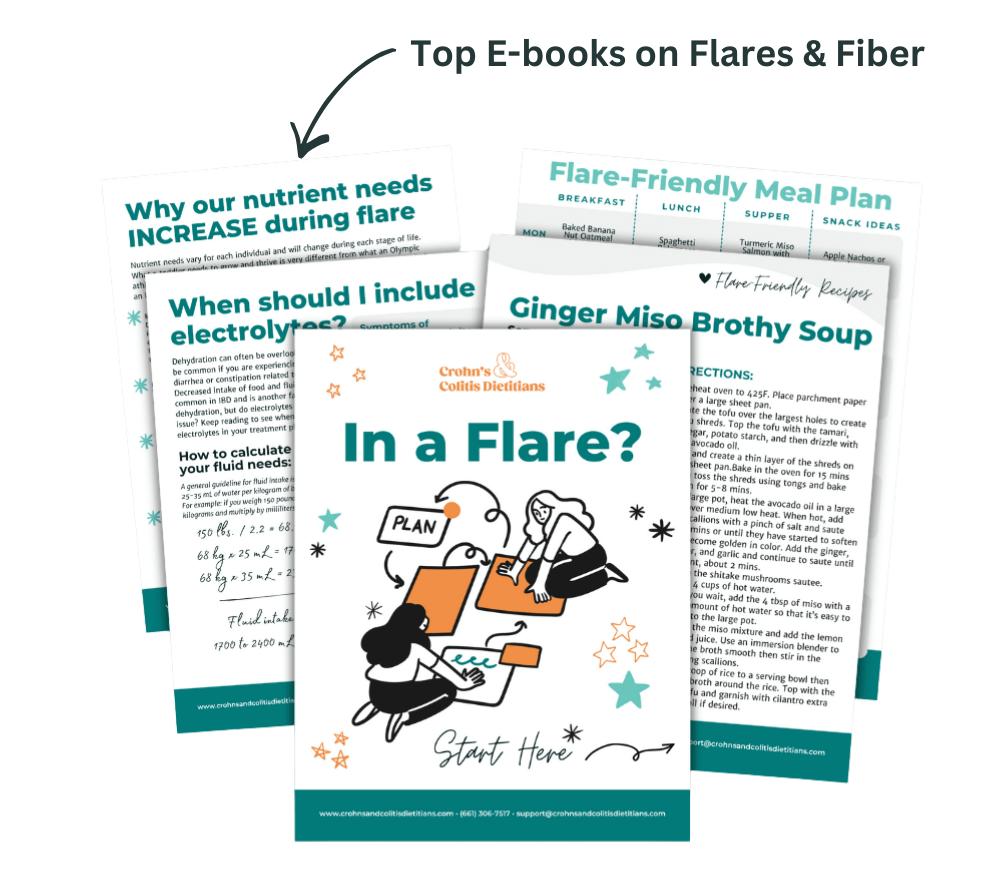
Be sure to check out our In a flare? Start here ebook for gut-friendly tips!
References
- Brotherton CS, Martin CA, Long MD, Kappelman MD, Sandler RS. Avoidance of Fiber Is Associated With Greater Risk of Crohn’s Disease Flare in a 6-Month Period. Clin Gastroenterol Hepatol. 2016 Aug;14(8):1130-6. doi: 10.1016/j.cgh.2015.12.029. Epub 2015 Dec 31. PMID: 26748217; PMCID: PMC4930425.
- Levenstein S, Prantera C, Varvo V, Scribano ML, Andreoli A, Luzi C, Arcà M, Berto E, Milite G, Marcheggiano A. Stress and exacerbation in ulcerative colitis: a prospective study of patients enrolled in remission. Am J Gastroenterol. 2000 May;95(5):1213-20. doi: 10.1111/j.1572-0241.2000.02012.x. PMID: 10811330.




THANK YOU for making so much good info available, free of charge. I have learned so much, just reading your posts/ blogs. It’s encouraging me more than you could ever know, as I’ve been from doctor to doctor with nothing to show but more bills and prescription meds that made me worse. So finding your website has been a godsend! It’s appreciated ✌️
Stacy thank you!! This means a lot to me. Here for you always.
This has been so informative
Thank you so very much .
I love reading these blogs they are so helpful.
Thank you Angela!