Sleep is a basic human need, yet in the non-stop world we live in, it’s somehow become seen as somewhat of a luxury.
The bottom line is that we need good quality sleep to function at our best, be healthy and live well. Yet the Center for Disease Control and Prevention has reported that up to 70 million Americans have chronic sleep problems.
Chronic sleep issues are not something to be taken lightly. Poor sleep long-term can lead to everything from heart failure and stroke, to depression and a reduced immune system, to a knock-on effect on your appearance.
And when you throw IBD into the mix with sleep issues, it gets even more serious.
Sleep and IBD have a complex relationship that’s not yet fully understood. What we do know is that overall wellbeing is key in keeping IBD symptoms and flare-ups under control, and sleep is no exception.
It’s important to familiarise yourself with the key facts and figures on sleep and IBD and get equipped with the knowledge to help keep your IBD under control.
Sleep disturbances: a contemporary endemic?
With such a large proportion of Americans suffering from sleep problems, it begs the simple question: why?
It’s been found that sleep duration has decreased over the last 50 years, impacting on our health and quality of life. Let’s take a stab in the dark and say this is down to the nature and pressures of modern life.
It can be challenging to switch off when we’re ruled by the internet and addicted to our devices. The world is constantly at our fingertips, and many of us have replaced bedtime reading with bedtime scrolling.
Studies have also found that “increasing work demands and shifting work schedules are major causes for chronic sleep deficiency in the general population.” We expect everywhere to be open and available 24/7 in the contemporary age, and email and instant messaging have made it far too easy for managers to communicate with their team at all hours.
The lines between being “on” and being “off” are blurred.
Sleep issues in IBD sufferers
When we look at sleep statistics of IBD sufferers, it’s clear that sleep issues are a common issue.
Studies suggest that 75% of patients with IBD have sleep disturbances – is this a coincidence, or is there more at play?
Whether you have IBD or not, sleep is paramount for good health and a happy mindset. But bad sleep can also have a direct impact on inflammation.
This has extra implications for those with Crohn’s or Colitis and can lead to increased symptoms, daytime fatigue, and overall lower quality of life.
The connection between your gut and sleep
Poor sleep can affect the gut because our circadian rhythm is partially controlled by the peripheral GI system.
To put it simply, this means that our natural internal 24-hour clock is linked to our gastrointestinal system.
Explaining this connection in full can get pretty complicated, but what’s important to note is that studies have found that “Disruption of circadian physiology, due to sleep disturbance or shift work, may result in various gastrointestinal diseases, such as irritable bowel syndrome, gastroesophageal reflux disease or peptic ulcer disease.” It can also have an impact on IBD symptoms.
Other factors that can affect your internal clock include exposure to light, your genes, and your diet.
IBD and sleep: chicken or egg?
While studies have shown that sleep impairment is a risk factor for active IBD disease or flare-ups, the direction of the relationship is still in question.
It’s been described as a chicken and egg situation – sleep issues can worsen inflammatory diseases, such as IBD, but it could also be that IBD is having a negative impact on sleep, therefore creating a vicious cycle.
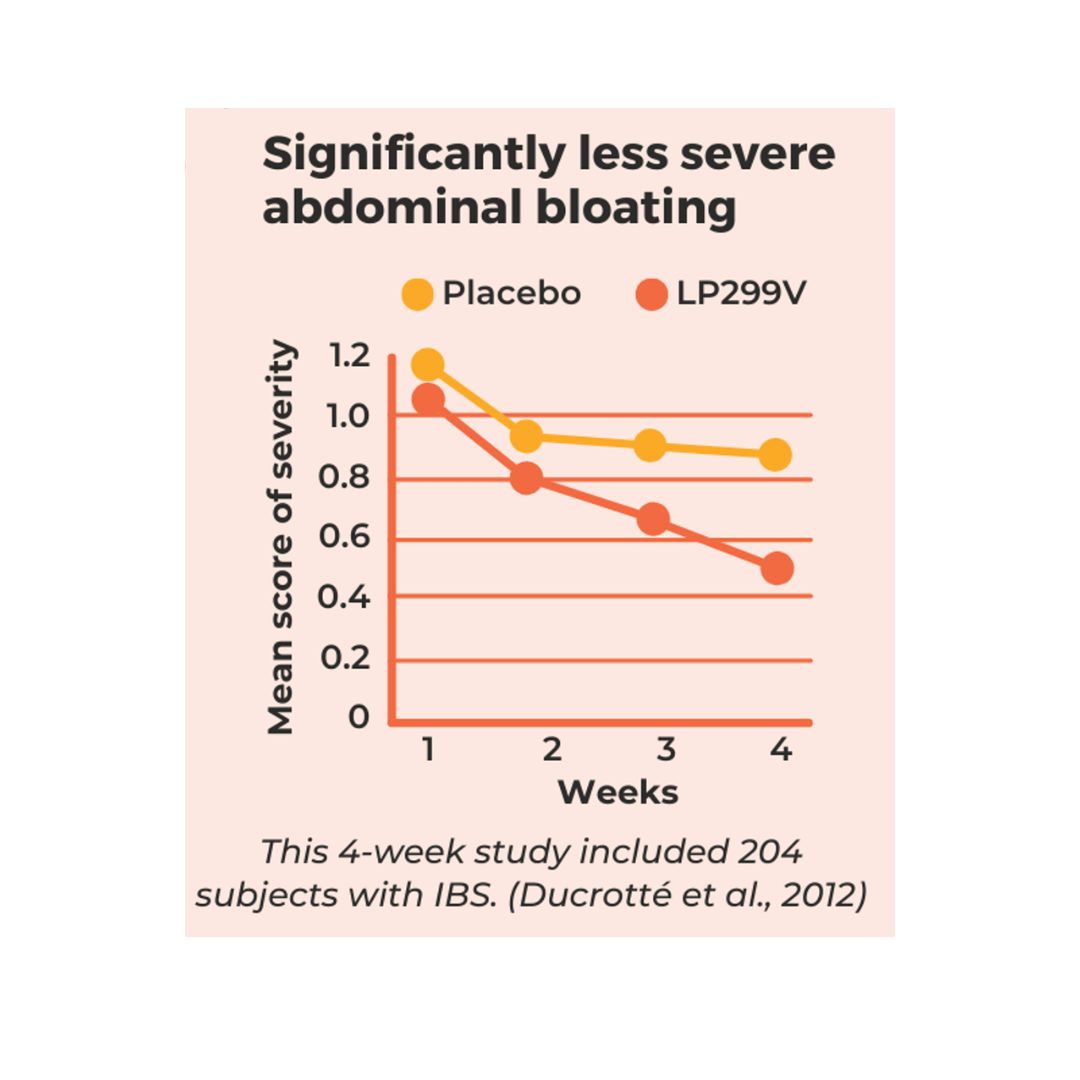
And IBD certainly does have a direct impact on sleep. Symptoms such as bloating, gas, abdominal pain, and an upset stomach can make it tough to get a decent rest, as can the stress that symptoms and flare-ups can bring about. Read more about coping with stress and flare-ups.
Symptoms and stress can result in disruption to sleep and your circadian rhythm, which in turn could lead to a worsening of symptoms. It’s a complicated and multi-layered relationship.
What happens to the gut during sleep?
Don’t be fooled – our bodies are not passive when asleep.
Countless vital functions and processes take place during your slumber – it’s a time for your body to restore and replenish itself.
Slow-wave sleep or SWS is considered to be the most restorative phase and when the most impact from immune regulation takes place.
SWS is seen as being a period of rest for the colon, and disruptions to this key stage of sleep can have a direct effect on the gut, including decreased mucosal integrity, and thus more inflammation and worsening symptoms.
On the flip side, good sleep can strengthen immune function and decrease proinflammatory cytokines. Ultimately, getting an adequate amount of deep sleep, or SWS, promotes a healthier gut, whereas sleep disturbances can worsen IBD symptoms.
Sleep tips for IBD sufferers
You don’t need to get bogged down by the ins and outs of biology, just keep in mind that good sleep can lead to better managed IBD.
With that said, let’s end with some simple tips for good sleep:
- Establish a bedroom routine that’s realistic and easy to stick to
- Keep your bedroom dark and cool
- Replace nighttime scrolling with reading a book
- Allow yourself time to wind down in the evening with relaxing activities
- Track your sleep patterns in a journal and relate them with your IBD symptoms
We hope this has given you a comprehensive overview of the complex relationship between sleep and IBD. As we said, you don’t need to become a biology expert, but having the right knowledge is an essential step in reaching that all-important symptom remission.
Nutritional support is also a key step to reaching symptom remission.
Our expert team of IBD dietitians are ready and waiting to give you the support and nutritional therapy you deserve – get in touch today.





0 Comments
Trackbacks/Pingbacks