The Centers for Disease Control and Prevention (CDC), states that roughly 3.1 million (1.3%) adults in the United States have an IBD diagnosis, while up to 15% of patients have an IBS diagnosis according to the American College of Gastroenterology (ACG). While these two gastrointestinal conditions may present themselves similarly, they are quite different for many reasons. Keep reading to learn more about how IBD and IBS are NOT the same conditions and why sometimes patients can get misdiagnosed with other conditions instead.
IBS Diagnosis: Are we missing something else?
What you need to know about IBS
Irritable bowel syndrome, also known as IBS, is commonly confused with Inflammatory Bowel Disease (IBD). Both IBD and IBS can present similarly to each other and can therefore lead to a misdiagnosis.
Because IBS has very similar symptoms to other conditions which we will explore in a bit, it is important to rule out other conditions that can mimic this syndrome. In fact, IBS and IBD are not the same. Each condition is treated both medically and nutritionally differently.
But, how is it different?
How is IBS different from IBD?
The first clue is hidden in the name! IBS is an irritable bowel syndrome versus an inflammatory disease. IBS is a functional bowel disorder, meaning it doesn’t cause structural damage. A wide variety of symptoms are common with IBS, including abdominal pain, bloating, and change in bowel habits.
There are four overarching types of IBS that doctors will classify patients as depending on the predominating symptoms.
Types of IBS:
- IBS-D: Diarrhea type
- IBS-C: Constipation type
- IBS-M: Mix of diarrhea and constipation
- IBS-U: Unclassified
Each type presents a little differently and has slightly different treatment options.
Symptoms of IBS are thought to “come and go” for a period, just like IBD. IBS can also vary dramatically in the intensity of the symptoms. But some patients may experience very mild symptoms and others’ quality of life can be compromised by debilitating symptoms. It may also be more prevalent than what is currently known; it seems that more people may have this syndrome without seeking medical care.
Frustration and stress are all too common and just like IBD, can be tough committing to plans due to the uncertainty of this syndrome. Interestingly, IBS symptoms are also common in patients who have IBD.
Misdiagnosis and the differential diagnosis of IBS
Getting misdiagnosed with IBS is all too common for people with IBD and other conditions that mimic this syndrome. While IBS can still be a diagnosis on its own, it’s important to understand the differential diagnosis.
Sometimes, when a colonoscopy is performed without biopsies, there can be a missed diagnosis of microscopic colitis (type of IBD) and instead an incorrect diagnosis of IBS.
How is IBS diagnosed?
Medical doctors can properly diagnose a patient with IBS using diagnostic tools and by using the Rome lV criteria. The Rome IV criteria looks at bowel habits along with abdominal pain and other symptoms including bloat, visceral hypersensitivity (pain within the organs), constipation and/or diarrhea, excess gas, and nausea.
IBS is diagnosed by looking at the person’s symptoms and ruling out other conditions that can mimic IBS. So let’s take a look at some of the red flags and get a better understanding of what these conditions are.
Other conditions that can look like IBS (Red Flags):
- Inflammatory bowel disease (IBD)
- Colon cancer
- Pelvic floor disorders
- Endometriosis
- Bile acid malabsorption
- Celiac disease
- Others
Let’s discuss each of these in a bit more detail to learn how they overlap in symptoms and presentation with IBS.
What is inflammatory bowel disease (IBD)?
Ah, the question that most of us with IBD try to answer in one sentence but know that it’s almost nearly impossible to do so. Right?!
Well, let’s see how we can break this down in simpler terms so it is easily digestible (see what I did there? 🙂). IBD is not the same as irritable bowel syndrome and it is also not called irritable bowel disease.
Inflammatory Bowel Disease is an umbrella term that is further broken down into 3 different conditions including Crohn’s Disease (CD), Ulcerative Colitis (UC), and Microscopic Colitis (MC). In addition, there are two types of microscopic colitis including lymphocytic colitis and collagenous colitis which we will discuss in further detail.
Inflammatory bowel disease can be diagnosed with the help of certain tests including stool and blood tests. Colonoscopies and upper endoscopies are also common diagnostic tools. According to the Crohn’s and Colitis Foundation, radiology scans and/or diagnostic imaging can be used to diagnose IBD, especially in more difficult areas to observe and diagnose.
Types of IBD
Let’s break down the types of IBD and see how they differ from each other.
Crohn’s Disease:
- Inflammation can occur anywhere from the mouth to the anus
- Can also be called ileitis
- Strictures and narrowing of the intestine can occur
- Presents itself as “skip lesions” and has a cobblestone appearance under a scope.
- Symptoms can include fever, blockages, diarrhea, abdominal pain/cramping, fistulas, ulcers, mouth sores, and narrowing of the intestines. There may be other symptoms that can be present
- Inflammation can be found in deeper layers of the bowel
Ulcerative Colitis:
- Inflammation is only present in the colon (large intestine)
- Ulceration can be found throughout the colon
- Can increase a person’s risk of colon cancer
- Symptoms can include fever, diarrhea with blood, abdominal pain/cramping, rectal bleeding, ulcers, urgency, mouth sores, weight loss, and fatigue. There may be other symptoms that can be present
- Toxic megacolon if inflammation is not treated
Lymphocytic Colitis:
- Type of Microscopic Colitis
- Microscopic evidence of inflammation
- Watery (non-bloody) diarrhea that tends to be chronic
- Symptoms can include cramping and abdominal pain along with watery diarrhea. Nausea, dehydration, fatigue, bloating, and joint pain. There may be other symptoms that can be present
- Can be mistaken for IBS
- White blood cells are increased in colon tissue
Collagenous Colitis:
- Type of Microscopic Colitis
- Microscopic evidence of inflammation
- Watery (non-bloody) diarrhea that tends to be chronic
- Symptoms can include cramping and abdominal pain along with watery diarrhea. Nausea, dehydration, fatigue, bloating, and joint pain. There may be other symptoms that can be present
- Can be mistaken for IBS
- A thick layer of collagen or a type of protein is present in colon tissue
It can get a little confusing and it’s always best to work closely with a gastroenterologist to get an appropriate diagnosis!
What is colon cancer?
Colon cancer is a type of cancer that occurs in the colon, also known as your large intestine. This type of cancer is produced by a polyp within the colon. Because colon cancer is common in the United States, it is recommended for people to get screened at age 45. For those with an immediate family member who was diagnosed with colon or rectal cancer, it is recommended to begin screening at age 35.
Signs and symptoms of colon cancer:
- Blood in the stool
- Involuntary weight loss
- Abdominal pain/bloat
- Change in bowel habits (constipation/diarrhea)
- Fatigue
- Nausea and/or vomiting
Because it is possible to have colon cancer and not experience symptoms, don’t shy away from those screenings!
As we can see, colorectal cancer shares many common symptoms with both IBS and IBD. While having blood in the stool is a red flag, hemorrhoids are also common and unfortunately are also diagnosed without a proper evaluation in some. So it is crucial to know the source of bleeding when a person is experiencing any kind of GI bleed.
What are pelvic floor disorders?
Pelvic floor dysfunction is when a person has difficulties with relaxing the muscle within the pelvic floor region to have both a bowel movement and to urinate. Those who have pelvic floor disorders have difficulties with emptying their bowels such as straining to use the bathroom, painful intercourse, and even rectal leakage. Some may receive a misdiagnosis of pelvic floor dysfunction for irritable bowel syndrome due to their common presentation(s). This is true with having irritable bowel syndrome-constipation type or IBS-C.
While treating pelvic floor dysfunction is an important part of any of the GI conditions we are discussing in this article, a proper diagnosis is imperative to direct overall treatment.
What is Endometriosis?
Endometriosis is described as having tissue on the outside of the uterus and located within the pelvic region. This condition can lead to both pelvic pain and infertility (4). While endometriosis and IBS can also share similar symptoms, they are two completely different diagnoses. However, it is common for women who have endometriosis to also have IBS. In fact, patients who experience bowel endometriosis (one of the three subtypes of endometriosis) can experience symptoms such as diarrhea, abdominal pain, constipation, and bloat (4).
What is Bile Acid Malabsorption?
Bile acid malabsorption, also known as BAM, is described as having chronic diarrhea when there is a build-up of bile acids. About one-third of patients with BAM also have the IBS-D subtype (5). The current treatment for bile acid malabsorption includes bile acid sequestrants and focuses on lower-fat foods to help decrease the number of bile acids. Since BAM can look very similar to IBS-D, it can be overlooked by clinicians and the person may not receive proper treatment.
What is Celiac Disease?
Celiac disease, according to the Celiac Disease Foundation, is when gluten is ingested, and then the small intestine becomes damaged. Celiac disease is a common autoimmune disease where a person cannot tolerate gluten products including barley, wheat, rye, and triticale. When gluten is consumed by those who have celiac, the villi of the small intestine which helps absorb nutrients become damaged, causing malabsorption.
Symptoms can also include weight loss, anemia, bloat, fatigue, diarrhea, and other symptoms. Neurological conditions including cerebellar ataxia (poor coordination and gait instability) can also occur in patients who have celiac disease since gluten can damage a portion of the brain, the cerebellum (6).
Treatment of celiac disease is following a life-long gluten-free diet. Because celiac disease can show up differently for everyone, it is important that patients are asked specific questions, beyond digestion. Diarrhea can also be a hallmark symptom of some celiac disease patients and can be overlooked and misdiagnosed with IBS-D.
Key Takeaways
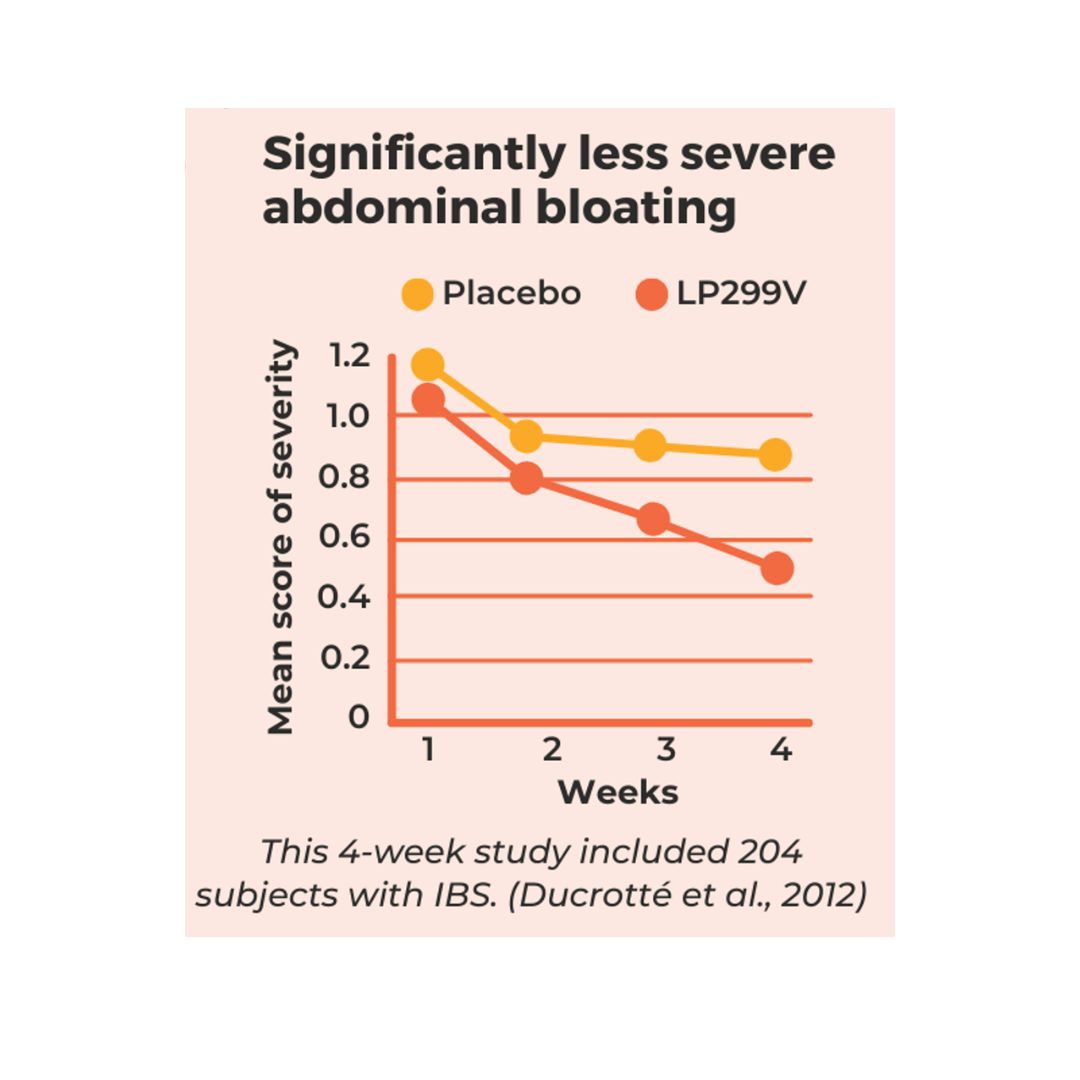
As mentioned previously, IBS is a functional bowel disorder that can be diagnosed through multiple diagnostic tools and criteria. Treatment for IBS can include pharmacotherapy such as antispasmodic medication, cognitive behavioral therapy (CBT), and trialing a 3-phased low FODMAP diet. In fact, there is no known cause of IBS. However, there are conditions that can lead to an IBS diagnosis including changes in the gut microbiota and immune system. There are many conditions that can mimic IBS as mentioned above along with other diagnoses including endocrine disorders, pancreatic exocrine insufficiency, small intestinal bacterial overgrowth (SIBO), and diverticular disease. It is important to look out for the red flags when having a diagnosis of IBS to avoid being misdiagnosed and getting to the root of the problem.
If you are seeking an appropriate diagnosis, make sure to build a team of practitioners that you trust. We can help with this process by coordinating your care and helping you navigate the process. Contact us today to determine ways we can help and support you!
References
- Hempel, KA., Sharma, AV. (2022). Collagenous And Lymphocytic Colitis. StatPearls [Internet]; 2022 Jan. https://www.ncbi.n1m.nih.gov/books/NBK41100/
- Fine, KD., Do, K., Schulte, K., Ogunji, F., Guerra, R., Osowski, L., McCormack, J. (2000). High prevalence of celiac-sprue-like HLA-DQ genes and enteropathy in patients with the microscopic colitis syndrome. The American journal of gastroenterology. 95(8):1974-82. https://doi.org/10.1111/j.1572-0241.2000.02255.x
- Bohr, J., Tysk, C., Eriksson, S., Abrahamsson, H., and Järnerot, G. (1996). Collagenous colitis: a retrospective study of clinical presentation and treatment in 163 patients. Gut. 1996;39(6):846-851. https://doi.org/10.1136/gut.39.6.846
- Tsamantioti, ES., Mahdy, H. (2022). Endometriosis. StatPearls [Internet]. 2022 Jan. https:// https://www.ncbi.nlm.nih.gov/books/NBK567777/
- Marasco, G., Cremon, C., Barbaro, MR., Falangone, F., Montanari, D., Capuani, F., Mastel, G., Stanghellini, V., and Barbara G. (2022). Pathophysiology and Clinical Management of Bile Acid Diarrhea. Gastroenterology & Hepatopancreatobiliary Medicine. 11(11),3102. https://doi.org/10.3390/jcm11113102
- Mearns, ES., Taylor, A., Craig, KJT., Puglielli, S., Cichewicz, AB., Leffler, DA., Sanders, DS., Lebwohl, B., and Hadjivassiliou, M. (2019). Nutrients. 11(2):380. https://doi.org/10.3390/nu11020380




0 Comments
Trackbacks/Pingbacks