5 Myths About Ulcerative Colitis
What is Ulcerative Colitis?
There are two types of IBD and Ulcerative Colitis (UC) is the most common form of Inflammatory Bowel Disease. Crohn’s Disease is also under the inflammatory bowel disease (IBD) bracket, shares similar symptoms to UC, and can affect anywhere in the gastrointestinal tract. It is more often found in the small intestine and can affect all layers of the intestinal wall.
Ulcerative colitis is characterized by inflammation in the large intestine (colon) and/or the rectum. The peak age of diagnosis is 30-40 years of age and is more common in males. “Approximately 1.6 million Americans currently have Crohn’s disease or ulcerative colitis. As many as 70,000 new cases of IBD are diagnosed in the United States each year” (1).
Colitis is an immune system dysfunction. In people without an autoimmune disease, the immune system protects the body against disease. But with UC, the body’s white blood cells attack the intestinal wall causing inflammation and ulcers.
Symptoms of UC include:
- Diarrhea (often with blood)
- Mucus
- Abdominal pain
- Weight loss
- Joint pain
- nausea/vomiting
- Decreased appetite
- Nutrient deficiencies
- Fatigue
Risk Factors of UC are:
- Age – the rate of UC is highest in people 15-30 and over 65 years of age
- Family History – if a close family member has UC, there is a 30%+ chance of developing it
- Ethnicity – Those of Ashkenazi Jewish descent have the highest rates of UC
- Of note: Environmental risk factors are not yet known, but many potential risk factors have been studied like smoking, antibiotic use, diet, non-steroidal anti inflammatory use, and appendectomy
There can be a lot of misconceptions about UC because so many of the above symptoms cannot be seen. Cue the line we’ve heard too many times to count… “But you don’t look sick!?”
IBD is an invisible illness, which is why it’s important to work with your healthcare provider to determine the best plan of action for your care.
At Crohn’s and Colitis Dietitians we want to provide you with the most evidenced-based information to help you understand the truth about this disease. No matter where you are in your IBD journey, we are dedicating this post to you. Today, this blog will debunk the myths about ulcerative colitis and only provide you with science-based facts.
5 Myths About Ulcerative Colitis
Let’s start separating fact from fiction today about ulcerative colitis! See the 5 Myths About Ulcerative Colitis below to learn the truth about IBD.
5. You should never have caffeine with Ulcerative Colitis

There is no doubt about it that certain foods and beverages have the potential to trigger uncomfortable gastrointestinal symptoms like urgency, diarrhea, bloating, abdominal pain, and more. However, that doesn’t mean you can never have that food item again.
Caffeine, more specifically, coffee, is a common beverage that is very much enjoyed in society, but can cause some unwanted symptoms if you have IBD. If you consume coffee and notice an uptick in symptoms, consider decreasing the serving size or take a break from it for awhile to see if symptoms improve.
Another lower caffeine option you may want to consider is to add green tea or matcha to your day. Green tea and matcha contain antioxidants that help fight cell damage in the body. They both also contain an amino acid called L-theanine. L-theanine is said to help decrease stress and anxiety and improve focus
Learn more about coffee and Ulcerative Colitis here.
4. If you have gastrointestinal symptoms you are not in remission
Unfortunately, some people with inflammatory bowel disease will still experience symptoms even when they have achieved clinical remission. Clinical remission is when there is no longer inflammation present.
So, why would someone still have symptoms? Approximately half of those with Crohn’s Disease or Colitis can experience symptoms of irritable bowel syndrome. If you are curious about IBS vs IBD, check out this blog post.
Symptom management and improved quality of life can be helped with a specific nutrition plan and lifestyle changes that an IBD dietitian can help with.
3. You will feel fatigued for the rest of your life
We totally understand that it can feel this way when you are fighting a flare or are on the path to healing. However, fatigue is something that can be improved over time.
Common reasons for fatigue in IBD include:
- Decreased food intake
- Inflammation in the body
- Nutrient deficiencies
- Dehydration
- Lack of sleep
Staying up to date on bloodwork, taking medication as prescribed, and stress management are a few things to focus on to fight fatigue. Read more about Ulcerative Colitis Fatigue here.
If you are looking for ways to improve the above symptoms, read our blog post here.
2. The Carnivore Diet will cure my IBD

This diet has been receiving a lot of attention lately and can leave someone wondering…will the Carnivore Diet cure my Ulcerative Colitis?
First off, what exactly is the Carnivore Diet? It is a diet high in animal protein with no carbohydrates allowed. Red meats, poultry, dairy products, fish, and organ meats make up a large portion of the diet leaving no room for other essential nutrients like fiber, antioxidants, and not to mention…fun. Some people may experience less gut symptoms following the carnivore diet (as it is devoid of fiber), but no irritation does not mean no inflammation.
Second, research shows that a diet rich in fiber is health promoting. Whereas, a diet high in animal proteins increases the risk of intestinal disease therefore altering the gut microbiome (3). Lastly, a diet high in red and processed meats has been linked to colon cancer (4).
The truth is, there is no cure for IBD. There is anecdotal evidence spouted about the Carnivore Diet on social media often, and little (if any) to be said about any positive effects it can have on one’s IBD in the scientific literature.
Related: Protein Needs in Ulcerative Colitis
1. People with UC should eat a low fiber diet
We understand that fiber mixed with IBD can be a scary thing, and we are here to tell you that this doesn’t have to be the case.
The Crohn’s and Colitis Dietitians teach people to understand the difference between triggering irritation and inflammation. A certain food may cause symptoms, but that doesn’t mean it’s triggering inflammation. The opposite is also true. There are specific dietary patterns that contribute to inflammation and people may experience limited symptoms.
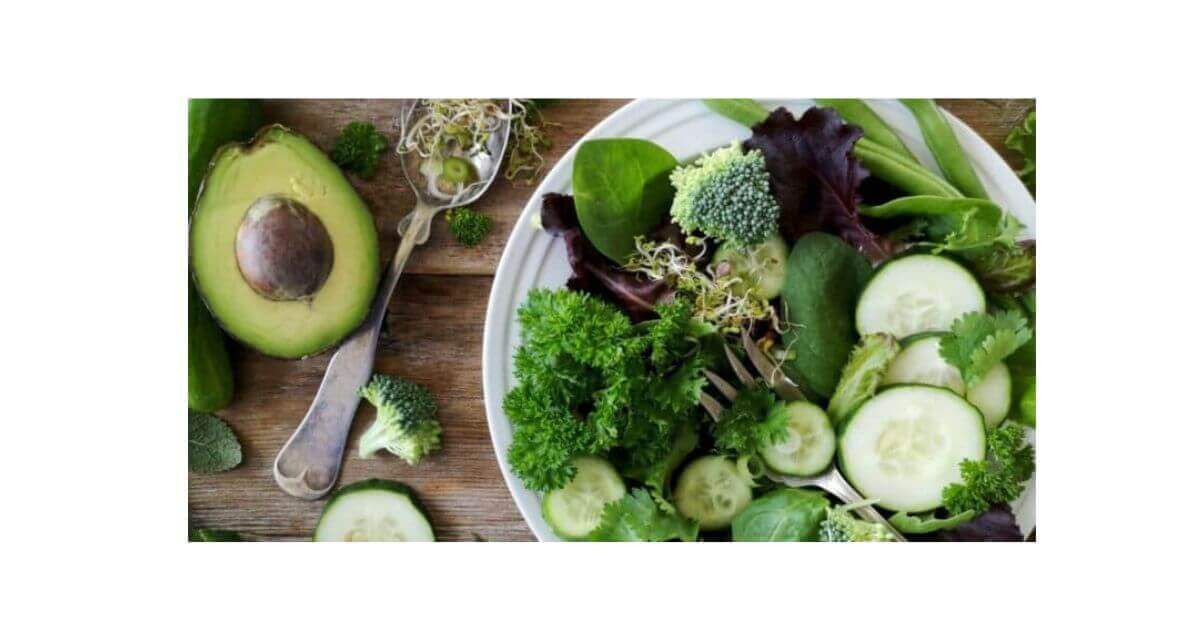
Individuals with inflammatory bowel disease who continued to follow a higher fiber diet were 40% less likely to flare! (2). Fiber helps the body create a short-chain fatty acid called butyrate which helps aid in inflammation reduction, supports the immune system, and helps to repair the gut lining. We want to ensure we are including fiber instead of reducing it.
If you find you get abdominal pain or other gastrointestinal symptoms while trying to increase fiber try these tips:
- Go low and slow – start with smaller portions of fibrous foods to build your tolerance. Try ¼ cup serving and slowly increase to what works for you
- Change the particle size – blend or puree foods to make it easier to digest. Examples include smoothies, pureed fruits like applesauce, or pureed soups
- Cook it up – tolerance to raw veggies may be low in the beginning. Consider sauteing, baking, or roasting vegetables
Of course, you need to consider the entire diet when it comes to health and there are plenty of things you can add to your day to see benefits. If you are looking for a more comprehensive ulcerative colitis food list check out our blog!
Related: Smoking and Ulcerative Colitis
Key takeaways
With all the information on the internet, it can be overwhelming to decipher fact from fiction. Asking if the information you read or see online has evidence or if they are only personal statements can challenge the viewer to look for another source if something sounds too good to be true.
We hope you were able to find some clarity after reading this blog on myths about ulcerative colitis.
If you need further support on your IBD journey and are wanting more information on what type of programs we offer, we would be happy to set up a free discovery call with you here!
References:
- Crohn’s and Colitis Foundation of America. (2014). The facts about inflammatory bowel diseases – Crohn’s & Colitis Foundation. Retrieved from https://www.crohnscolitisfoundation.org/sites/default/files/2019-02/Updated%20IBD%20Factbook.pdf
- Brotherton, C. S., Martin, C. A., Long, M. D., Kappelman, M. D., & Sandler, R. S. (2015, December 31). Avoidance of fiber is associated with greater risk of crohn’s disease flare in a 6-month period. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4930425/
- Cai, J., Chen, Z., Wu, W., Lin, Q., & Liang, Y. (2022). High animal protein diet and gut microbiota in human health. Critical reviews in food science and nutrition, 62(22), 6225–6237. https://doi.org/10.1080/10408398.2021.1898336
- Farvid, M. S., Sidahmed, E., Spence, N. D., Mante Angua, K., Rosner, B. A., & Barnett, J. B. (2021). Consumption of red meat and processed meat and cancer incidence: a systematic review and meta-analysis of prospective studies. European journal of epidemiology, 36(9), 937–951.



When I left the Hospitol with diagnosls of Ischemic colitis after passing and a low fiber in hand . It helped sort of but my life is so unsure and paper pants.I am a wreck
Please reach out to work with us for this.