Have you ever wondered about smoking and ulcerative colitis?
Living with ulcerative colitis can feel rough when you’ve got unpredictable flare-ups. Ulcerative colitis (UC) is a chronic disorder of the digestive system, specifically the colon and rectum, characterized by persistent inflammation, bleeding, abdominal pain, urgency, and disruptions to your daily life.
For many, the term ulcerative colitis evokes not only physical symptoms but also anxiety about active disease or worries about increased risk of developing complications.
When symptoms feel dire, this can often lead people to feel desperate for answers and willing to try anything. As patients ourselves, we can relate to this feeling. As practitioners though, we have seen the dangers of trying anything and everything.
Our purpose as a company is to provide credible answers to common questions we get and provide those with IBD like us with hope and more clarity.
If you are someone that has gone down the path of trying at all – you may have come across more contreveral topics like smoking and ulcerative colitis. While the dangers and risks of smoking are far too high to outweigh any positive benefits, there have been some interesting studies that point to the need to look into the use of nicotine.
Smoking and Ulcerative Colitis
Let’s unpack what we know about the relationship between smoking and Ulcerative colitis. Including:
- What happens when you smoke—the mechanics, the chemistry, the effects of cigarette smoke and effects of nicotine, both systemic and local
- How those factors smoking exerts on the digestive tract and immune system may influence active UC
- Scientific insights: studies show that smokers with UC sometimes show paradoxical patterns, including a strange protective effect or protection against UC
- The research suggests that nicotine might help some ulcerative colitis symptoms in limited contexts—such as with nicotine patches or nicotine enemas
- Finally, we will review the best treatment paths for ulcerative colitis
If you are looking for nutrition focused blogs- check out foods for ulcerative colitis list or if you’d like to learn more about remission – check out our blog on the the 4 different types of remission and how they are defined.
What Happens When You Smoke
When you inhale cigarette smoke, a complex mix of thousands of chemicals enters your lungs and eventually your bloodstream—including nicotine, carbon monoxide, tar, heavy metals, reactive oxygen species, and pro-inflammatory compounds. Here’s how these effects of smoking play out:
- Immediate Immune Responses
Smoking triggers changes in the immune system—raising certain pro-inflammatory cytokines, dampening others, and altering how immune cells behave. Some studies note shifts in regulatory T cells, macrophages, and neutrophil activation as systemic effects of inflammatory bowel disease IBD interact with smoking-induced immune modulation. - Impact on Blood Vessels & Nitric Oxide
Smoking reduces levels of nitric oxide, a vasodilator that supports healthy blood flow and mucosal healing in the gut. Reduced nitric oxide may impair the integrity of the mucosal barrier—potentially worsening UC flare-ups. - Oxidative Stress & Tissue Damage
Cigarette smoke also created additional free radicals, leading to oxidative damage in intestinal tissues. In UC—where the colon lining is already inflamed—this oxidative stress can amplify mucosal injury. - Altered Gut Microbiome & Barrier Function
Smoking can also have a negative impact on the microbiome and ultimately leading to impaired tight junctions in the intestinal mucosa, further compromising barrier function and potentially exacerbating UC symptoms. - Effects of Nicotine
Some studies show that nicotine may have some short-term anti-inflammatory effects and a more positive effect on motility. These potential benefits still need to be explored further. Smoking inevitably comes bundled with toxicants that overshadow any prospective benefits.
How Does Smoking Affect Ulcerative Colitis
While smoking isn’t something we recommend, it’s notable that there have been studies with interesting findings around smoking and Ulcerative colitis.
1. Can smoking have a protective effect against developing UC?
Paradoxically, some studies show that smoking is associated with a reduced risk of developing ulcerative colitis compared to non-smokers. Correlation studies don’t always indicate strong relationships, but it does point to something that should be further explored.
There could be a strange protective effect—perhaps owing to immunomodulatory effects of nicotine or other components. However, this protection against UC in epidemiological terms is not a treatment strategy—but rather an observed association.
2. Nicotine may have a small positive impact active UC
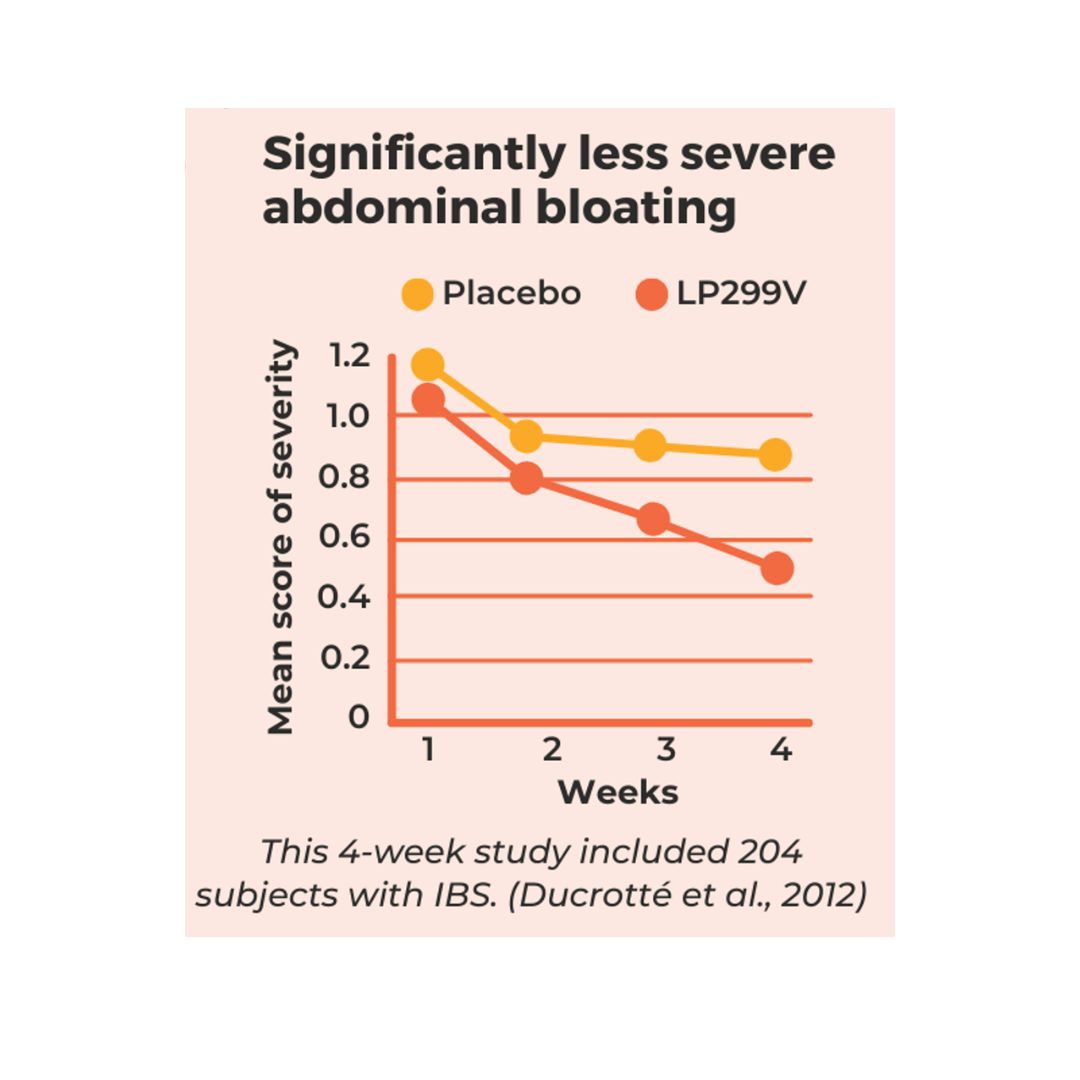
Some studies suggest that nicotine influences inflammatory pathways—potentially modulating the immune response and reducing colon inflammation. For instance, trials using nicotine patches or nicotine enemas in patients with mild-to-moderate active UC have shown modest improvement in symptoms for some individuals.
3. The risks and side effects far outweigh any benefit
Even with that limited data suggesting benefit from nicotine patches or nicotine enemas, the side effects are significant—and the broader context is clear: smoking introduces serious, life-threatening risks. Cardiovascular disease, lung cancer, chronic bronchitis, decreased nitric oxide, worsened oxidative stress, impaired immunity, and other harms strongly overshadow any transient GI benefit.
Moreover, chronic smoking may worsen the overall course of IBD via systemic inflammation and compromised healing. So while smokers with UC may sometimes—even biologically—experience different symptom trajectories, smoking is not an acceptable or safe therapeutic choice.
4. Environmental factors and exacerbation
Smoking is a classic environmental factor in IBD. As such, it not only influences disease risk but also may exacerbate GI symptoms during flares.
Combined with poor blood flow, impaired mucosal repair, and damaged barrier function, smoking tends to worsen active UC episodes. Again, any short-lived protective effect is far outweighed by the inflammatory and vascular damage of cigarette smoke.
5. Long-term smoking and IBD complications
Over time, smokers with IBD (even UC) face increased risk of developing colorectal dysplasia, colorectal cancer, extra-intestinal complications, and cardiovascular comorbidities. The balance is heavily skewed: short-lived gut benefit (if any) vs long-term systemic harm.
Is Smoking Good for Ulcerative Colitis?
Short answer: No.
While nicotine—in isolation and via controlled delivery—may have some modest beneficial effects on colon inflammation in active UC, the risks and side effects far outweigh any potential gain from smoking.
- Smokers with UC sometimes show milder disease or lower incidence of developing UC in epidemiological studies. But correlation is not causation.
- Nicotine patches or nicotine enemas can be studied under controlled settings. But they come with side effects and are nowhere near a standard of care.
- Effects of nicotine on the immune system are complex—studies show a mix of outcomes. And any temporary improvement is fragile and highly individual.
- Meanwhile, smoking introduces serious vascular, pulmonary, cancer, and systemic risks. It reduces nitric oxide, impairs healing, increases oxidative stress, damages microbiome and barrier, undermines immunity, and compounds comorbidities.
In essence, if someone asks, “Is smoking good for ulcerative colitis?”—the answer is: No. The few narrow findings of potential benefit from nicotine do not justify causing harm through smoking.
What’s The Best Treatment for Ulcerative Colitis
Here, we’ll explore key treatment options for ulcerative colitis, with concise explanation and context, always prioritizing safety, efficacy, and patient-centered care.
Medications to treat UC
Used for mild-to-moderate UC, these medications (e.g., mesalamine, sulfasalazine) target inflammation in the colon lining. They’re often first-line for maintenance and flare treatment. Side effects are generally mild but can include headache, bloating, nausea and joint stiffness.
Corticosteroids like prednisone or budesonide are powerful anti-inflammatory agents for moderate-to-severe flares (not long-term). They act quickly to suppress immune response. But side effects—like weight gain, osteoporosis, mood swings, glucose elevation—limit prolonged use.
For moderate to severe UC, often immunomodulator therapy, biologics or small molecule therapies are used. Surgery, while not typically a first line of therapy, is another treatment route for UC.
If you are someone struggling with getting enough food, experiencing weight loss or if you only have a few safe foods – these are signs of malnutrition and we know malnutrition can actually negatively impact how well your medications work and can increase symptoms!
If this is you, it’s important to get support from an IBD focused dietitian like us who knows how to treat IBD malnutrition. Feel free to book a call with us here.
Dietary Interventions for UC
If you’ve found our website, you are probably already somewhat aware of the importance on dietary support in Ulcerative colitis. When you work with IBD-focused dietitians (like us) we will practice medical nutrition therapy – which is nutrition designed to treat the IBD.
This means we will craft a strategy customized to you to help you expand your diet and reduce symptoms. We will also help guide you to the best strategies for supporting reduced inflammation and reduced risk of flare-up long-term.
If you are curious and want to know more about the strong evidence for why nutrition matters – check out our resources page! We have a great handout you can share with your providers on why nutrition matters. We also have many e-books with practical guidance on how to navigate IBD.



0 Comments
Trackbacks/Pingbacks