This post goes over how our gut health impacts other aspects of health- including cardiovascular and metabolic health. You can use the glossary below to refer to terms I mention in this module.
Glossary:
Metabolic syndrome/diseases– A cluster of conditions that often occur together including increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels.
Short Chain Fatty Acids (SCFA’s)- Our gut bacteria consume some of the leftover foods we eat. The most helpful gut bacteria consume fibers from our food and secrete SCFA’s or short chain fatty acids. SCFA’s have widespread helpful effects throughout the body including- gut repair, inflammation reduction, lowered blood glucose and many other helpful things that reduce our risk and can help in reversing metabolic syndrome.
Secondary Bile Acids– Bile acids help us emulsify or break down fats. In normal amounts, bile is helpful to us. High amounts of saturated fat, dairy and meats tend to increase bile production which a not so helpful bacteria called biophyla wadsworthia likes to consume. As this bacteria increases in population, it can cause problems and is linked to health issues.
Lipopolysaccharides (LPS)- Out of balance gut bacteria leads to higher levels of LPS. High levels of bacterially-produced lipopolysaccharides have been reported in T2 diabetes patients and seems to link with metabolic dysfunction and inflammation.
Metabolic Diseases & Gut Bacteria
Metabolic diseases occur when the body’s usual metabolic processes for storing and using energy are interrupted. The gut microbiome plays a large role in these processes. The foods we consume can help in reducing our risk of further cardiac risk and may help in reversing some of these interrupted processes.
A Normal Healthy Process
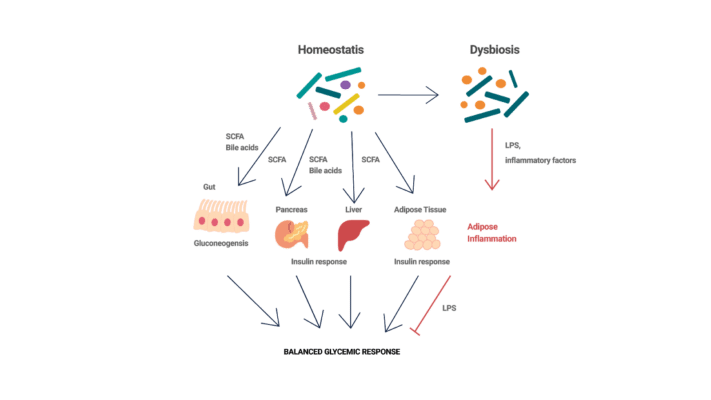
In a normal healthy metabolic process, gut bacteria produce short-chain fatty acids and molecules called secondary bile acids that help our body store or use energy appropriately.
For example, short chain fatty acids are released from helpful bacteria after they consume the fibers in our diet. The short-chain fatty acids (butyrate and propionate) then bind to receptors in the gut cells. The binding then triggers the release of metabolic hormones that lower blood glucose levels, reduce appetite and reduce overall inflammation (1,2).
An Out of Balance Response
When gut bacteria are out of balance, there are often high levels of bacteria that produce a pro-inflammatory molecule called lipopolysaccharide. High levels of bacterially-produced lipopolysaccharides have been reported in T2 diabetes patients, and obese and insulin-resistant mice.
Many studies have demonstrated that high levels of lipopolysaccharides can lead to inflammation of adipose or fat tissue which can drive insulin resistance and glucose intolerance (4,5).
Image inspired by: Suez et al. 20163.
The Bottom Line: What does this mean?
Including more plants in the diet is helpful for promoting more of this effect! Also, limiting the things that amplify metabolic disease will help in preventing and even reversing it.