From Food to Microbes
As we know, what we eat has a large impact on shaping our gut microbiome. But, how does that work?
Our digestive system transforms the leftovers of what can’t be fully digested (like fiber!) into by-products. By-products can be helpful, harmful, or somewhere in between. Helpful by-products are known as synbiotics.
This process starts in the mouth! For more on digestion, go here.
Eating to Nourish the Gut Microbiome
Since we don’t digest fiber and they pass through to the large intestine, the fibers we eat are consumed by gut bacteria. This process produces short-chain fatty acids (butyrate, acetate, propionate). These short-chain fatty acids pass through our intestinal cells and are then routed to the portal vein for passage to the liver. There is also communication to the brain during this process, allowing them to have systemic effects on the body. Intestinal cells use these by-products as fuel and for repair, helping to maintain a healthy, intact barrier. Short-chain fatty acids help with regulation of the immune response, regulation of mood and pain, reduction of inflammation (systemic and local), and regulating glucose stability and appetite. When we eat foods rich in plant-compounds and fiber we feed our gut bacteria, which creates less chance of pathogens and flare by creating helpful by-products to reduce inflammation. This environment supports stable remission and allows you to absorb more nutrients in this state.
.
When we do not eat fiber, skip meals, or limit the foods available we can starve off the helpful bacteria and create more dietary risk factors as unhelpful by-products create more inflammation. This creates a balance between the mucus-degrading bacteria and the fiber-degrading bacteria. We want to have more of the fiber-degrading bacteria so that the mucosal layer can stay healthy to decrease the chance of flare and maintain a healthy immune system.
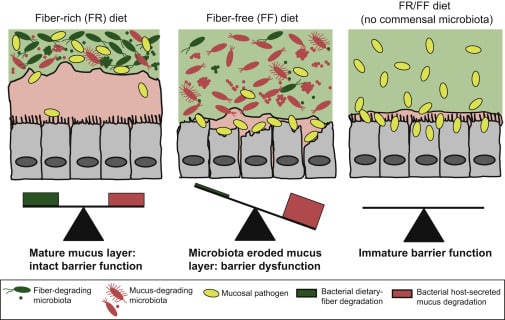
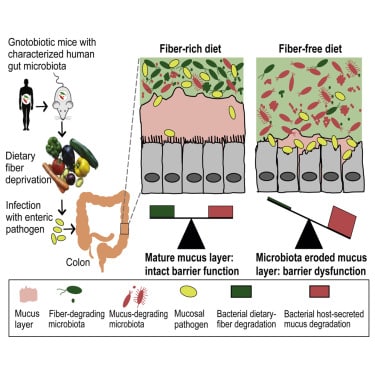
Mahesh S. et al., A Dietary Fiber-Deprived Gut Microbiota Degrades the Colonic Mucus Barrier and Enhances Pathogen Susceptibility, Cell, Volume 167, Issue 5, 2016, Pages 1339-1353.e21, ISSN 0092-8674, https://doi.org/10.1016/j.cell.2016.10.043.
Dietary factors that increase risk of flare
With all of this in mind, there are clear dietary factors that increase our risk of flare.
- Increased added and refined sugars (sodas, highly processed desserts, high fructose corn syrup)
- Increases inflammation and can cause more gas and bloating
- This would be in very large amounts, not the normal amount of sugar in a healthy diet
- Consumption of a Westernized diet
- High in animal meat
- Higher in fats (low in quality fats)
- High in dairy products
- High in refined sugars
- High in total protein intake
- High in processed meats (particularly nitrites)
- Consumption of certain fats
- Diet high in Omega 6’s (industrial oils, highly processed foods)
- Margarine
- Industrial oils with low smoke point (used over and over again)
- Decreased food for gut bacteria
- Low consumption of vegetable and fruits
- Low consumption of whole grains and fiber
- Low consumption of fish, low Omega 3’s
- Decreased consumption of fresh/raw fruits and vegetables
- Low fiber diet
- Specific risk factors for relapse/flare
- Fast food intake – 390% increased risk
- Higher intake of meats (not fish) – 320% increased risk
- Alcohol intake (1-3x/week) – 271% increased risk
- Sulphites (in processed foods, wine) – 276% increased risk
- Smoking
- Cessation is effective at reducing relapse by 65% (similar to immunosuppression therapy)
